YOUR JOURNEY TO RADIANT EYES BEGINS HERE
Specialized Cosmetic Eye Procedures Tailored Just for You
ABOUT DR. JORDAN
Dr. Jordan is a leading expert in ophthalmic plastic and reconstructive surgery. He graduated from the University of Toronto Medical School and completed advanced training at the Ottawa General Hospital, University of Iowa, and University of Utah. He has been with the University of Ottawa Eye Institute for many years and runs a successful private practice. As a full Professor of Ophthalmology, Dr. Jordan has trained many physicians and authored over 300 scientific articles. He is certified by the Royal College of Physicians and Surgeons of Canada and the American Board of Ophthalmology and is a member of several prestigious societies.








Upper Eyelid Surgery
Your eyes are a central feature of your face and significantly contribute to your attractiveness. As you age, your lower eyelids may start to sag or develop bags, making you appear tired or older than you feel. Lower blepharoplasty effectively addresses these issues, offering a rejuvenated look with minimal risk. This procedure is usually done under local anesthesia and is a simple, outpatient surgery performed by our skilled professionals.
LEARN MORELower Eyelid Surgery
Your eyes are the focal point of your face, crucial to your overall attractiveness. As we age, the upper eyelids can become droopy or baggy, giving a tired or older appearance. Upper blepharoplasty surgery offers a dual benefit: enhancing both function and aesthetics with minimal risk. This straightforward procedure, typically performed under local anesthesia, allows for a quick recovery as an outpatient. In the skilled hands of our experienced surgeons, you can achieve a youthful, refreshed look effortlessly.
LEARN MOREBROW ELEVATION
With age, the upper and lower eyelids become “droopy” or “baggy” in appearance, making one look “more tired” and “older” than they really are. Drooping eyebrows also contribute to these effects and in some patients are responsible for most of the “aged” or “tired appearance”. Brow lifting surgery provides both functional and cosmetic improvement with minimal risk of serious problems.
LEARN MOREBOTOX®
Facial Expressions are created by numerous facial muscles contracting at different times and to different degrees; causing the overlying skin to wrinkle and fold. Excess facial muscle contractions contribute to many undesired facial wrinkles and folds. Some of these wrinkles and folds may be cosmetically unattractive and misinterpreted as conveying anger, concern, sadness, or fatigue.
LEARN MORESOFT TISSUE FILLERS
Soft tissue fillers are commonly employed to enhance facial aesthetics by correcting various lines, folds, and volume loss. Over the years, the market has seen a range of fillers, including silicone, collagen, and autologous fat. These fillers can rejuvenate the skin by smoothing out wrinkles, plumping up areas that have lost volume, and enhancing facial contours, providing a more youthful and refreshed appearance. Advances in filler technology have also introduced hyaluronic acid-based fillers, which are popular for their natural-looking results and biocompatibility.
LEARN MORE







Upper Eyelid Surgery

Your eyes are the focal point of your face, crucial to your overall attractiveness. As we age, the upper eyelids can become droopy or baggy, giving a tired or older appearance. Upper blepharoplasty surgery offers a dual benefit: enhancing both function and aesthetics with minimal risk. This straightforward procedure, typically performed under local anesthesia, allows for a quick recovery as an outpatient. In the skilled hands of our experienced surgeons, you can achieve a youthful, refreshed look effortlessly.
LEARN MORELower Eyelid Surgery

Your eyes are a central feature of your face and significantly contribute to your attractiveness. As you age, your lower eyelids may start to sag or develop bags, making you appear tired or older than you feel. Lower blepharoplasty effectively addresses these issues, offering a rejuvenated look with minimal risk. This procedure is usually done under local anesthesia and is a simple, outpatient surgery performed by our skilled professionals.
LEARN MOREBrow Elevation

With age, the upper and lower eyelids become “droopy” or “baggy” in appearance, making one look “more tired” and “older” than they really are. Drooping eyebrows also contribute to these effects and in some patients are responsible for most of the “aged” or “tired appearance”. Brow lifting surgery provides both functional and cosmetic improvement with minimal risk of serious problems.
LEARN MOREBotox®

Facial Expressions are created by numerous facial muscles contracting at different times and to different degrees; causing the overlying skin to wrinkle and fold. Excess facial muscle contractions contribute to many undesired facial wrinkles and folds. Some of these wrinkles and folds may be cosmetically unattractive and misinterpreted as conveying anger, concern, sadness, or fatigue.
LEARN MORESoft tissue fillers

Soft tissue fillers are commonly employed to enhance facial aesthetics by correcting various lines, folds, and volume loss. Over the years, the market has seen a range of fillers, including silicone, collagen, and autologous fat. These fillers can rejuvenate the skin by smoothing out wrinkles, plumping up areas that have lost volume, and enhancing facial contours, providing a more youthful and refreshed appearance. Advances in filler technology have also introduced hyaluronic acid-based fillers, which are popular for their natural-looking results and biocompatibility.
LEARN MOREREAL STORIES, REAL RESULTS
The phrase “seeing is believing” rings especially true in the realm of cosmetic surgery. Our commitment to delivering exceptional results and personalized care is evident in the transformations we achieve. We trust these photos illustrate the careful attention to detail and artistic skill we apply to every procedure.

Our Philosophy
What do you notice first about someone’s face? Most often, it’s the person’s eyes. Eyes can tell you what another person is feeling – approval, amusement, anger, love, jealousy, confusion and agreement. “Eyes are windows of the soul,” it is said, and the focal point of the face.
What do people see when they look at your eyes? What do you see? The natural aging process, inherited traits, an injury or a blemish – any of these can alter your appearance.
To us you are a unique individual. Your eyes and your needs are different from those of anyone else and are our primary concern. We want to understand your needs, help you develop realistic expectations, and determine the right surgical plan just for you.
It is very important to us that we provide you with all the information you need – that none of your questions or requests go unanswered. Your satisfaction with the results of your surgery and with all the steps before and after surgery is our primary goal.
Dr. Jordan specializes in Oculoplastic Surgery which deals with problems affecting the eyelids, tear ducts and eye socket. He also has a special interest in cosmetic eyelid surgery and botulinum toxin injections, as well as soft tissue fillers.
INSIGHT NEWS LETTERS BY DR. JORDAN
Ptosis (pronounced “toe-sis”) refers to a drooping of the upper eyelid. The lid may droop only slightly or it may droop enough to partially or completely cover the pupil, restricting or obscuring vision.
Ptosis may be inherited. It can affect one or both eyelids, be present at birth or occur later in life. Ptosis which is present at birth is called Congenital Ptosis. If the ptosis develops with age it is referred to as Acquired Ptosis.
What causes Congenital ptosis?
Congenital ptosis is most often due to an under-development of the eyelid lifting muscle – “the levator”. Although usually occurring as an isolated problem, children born with ptosis may also have eye movement abnormalities, muscular diseases, lid tumors or neurological disorders. Congenital ptosis does not improve with time unless it was caused traumatically at the time of birth.
How is it treated?
The treatment for congenital ptosis is surgical in the overwhelming majority of patients. In determining whether surgery is advisable, an ophthalmologist specialized in treating droopy eyelids considers the individual’s age, the severity of the ptosis and whether one or both eyelids are involved. Measurement of the lid height, evaluation of the eyelids lifting and closing muscle strength and observation of the eye movements determine which surgical procedure is more appropriate.
The most common procedure involves advancing the under-developed levator muscle while the child is under general anesthesia. If the levator muscle has little or no function, the lid has to be attached or suspended to the brow so that the forehead muscle does the lifting (Brow Suspension).
Adult Ptosis
The most common type of adult onset ptosis is due to a weakening of the attachments between the levator muscle and the lid. This may occur as a result of the aging process, after cataract surgery or from an injury. Adult ptosis may also occur as a complication of other diseases involving the levator muscle or its nerve supply such as diabetes or myasthenia, or it may occur when movement of the levator muscle is restricted as may happen in the case of an eyelid tumor.
What are the Signs and Symptoms of Adult Ptosis?
The most obvious sign is a droopy upper lid. The patient may complain of peripheral visual loss or fatigue from attempting to elevate the droopy lid. Reading may be difficult as the ptotic lid tends to block the visual axis when the eye is looking down. Adults with ptosis will often tip their heads back to see past their eyelids or raise their eyebrows in an effort to raise their lids. If the ptosis is severe they may bump into things at a forehead level (cupboard doors).
How is Adult Ptosis Treated?
Treatment when necessary is usually surgical and is done as an outpatient under local anesthesia. It is important to do the surgery under local anesthesia when the patient is old enough to co-operate (usually over the age of 12). This gives the surgeon a better idea of how much to raise the eyelids. Postoperatively there is usually some mild lid swelling which settles over the first 2 weeks or so. The patients are generally quite relieved to have the visual obstruction removed.
What are the Risks of ptosis surgery?
Bleeding and infection are possible but extremely rare. Patients on Aspirin and anti-arthritic medication may be asked to stop these for a few days prior and post surgery to reduce the chance of bleeding and bruising.
Under or over correction can occasionally occur and if obvious, a suture adjustment may be required in the first to two weeks.
A temporary inability to fully close the eye after ptosis surgery is not uncommon and resolves in most over a few weeks. The eyelids do not remain “stuck open”. During this time period when the lids are not fully closing it is important to use lubricating drops and ointment to keep the cornea moist.
Summary
Ptosis in children and adults can be successfully treated with surgery to improve visual function as well as improve cosmetic appearance.
The drooping lid can affect visual development in an infant and if the lid is encroaching in the visual axis, an ophthalmic assessment is important to avoid the development of amblyopia.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.
Excess Eyelid Blinking
INTRODUCTION
Normal individuals have at least 3 different behavioral patterns of blink rate. The normal blink rate is higher during verbal conversation compared with rest, and slowest during reading. Blinks occur, on average, approximately 15 times per minute in the adult patient. Blinking is virtually absent at birth and increases steadily until adolescence, when it plateaus and is maintained throughout adult life. In an infant, blinking may occur as infrequently as one to two times per minute. Spontaneous blinking occurs even in blind eyes and is not dependent on visual stimulation.
The patient with excess blinking on one or both sides may have one of the following:
Anterior Segment irritation
Any disorder that produces irritation of the ocular surface or photophobia may be associated with an increased blink rate. For example, severe dry eyes, inturned eyelashes (trichiasis), iritis or scleritis, foreign bodies on the cornea or in the cunjunctial fornix (eyelash, sand, metal fragment from a power tool, etc.) may cause increased blinking.
Habit Spasms or facial tics
Habit spasms or facial tics are repetitive mannerisms of variable frequency involving any number of facial muscles. An eye-blinking tic most commonly presents in childhood as a rapid, exaggerated, coordinated contraction of the orbicularis oculi. Boys are more common only involved than girls and the increased blinking is usually bilateral. The blinking can be voluntarily controlled to some degree, but it often increases in frequency when the individual is bored, tired, or anxious. There may occasionally be other facial twitches present as well. There is little functional visual impairment, and the facial tic typically disappears spontaneously after a duration of weeks to years.
Myokymia
Myokymia is a localized muscle twitch in the eyelid. It is characterized by an involuntary, fine, muscle contraction involving a portion of the orbicularis oculi muscle or other facial muscles. It is often described as a flickering of one eyelid occurring intermittently throughout the day. It tends to occur in young ( 20’s – 30’s), healthy individuals and may last minutes, hour or days. There may be a history of excessive physical exertion, fatigue, lack of sleep, stress or excessive caffeine consumption. It may also be seen after almost any type of eyelid surgery.
Myokymia generally requires no treatment as it commonly resolves spontaneously. Obtaining adequate sleep, reducing caffeine intake and decreasing stress are helpful. If the twitches persist on a daily basis for several weeks, a mild muscle relaxant or an injection of botulinum toxin can be used. Botulinum toxin is extremely effective.
Aberrent Regeneration following Bells Palsy
With Bells Palsy, the facial nerve, loses function. During the regenerative or healing phase, the nerve often regenerates in an abnormal way. This aberrant regeneration is manifest in several ways. The upper and lower eyelid on one side may partially close or twitch during conversation and chewing. Alternatively, there may be excess tearing while chewing food.
The most effective treatment for aberrant regeneration involves botulinum toxin injections. Botulinum toxin injected in minute quantities into the abnormal twitching muscle fibers, will significantly weaken the muscle fibers and decrease the eyelid closure and eyelid twitching. By injecting botulinum into the lacrimal gland the excess tearing during chewing can also be improved.
Benigh Essential Blepharospasm
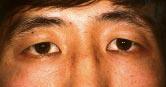
The term “Blepharospasm”, literally means spasm of the eyelids, and has numerous causes. For example, a foreign body on the cornea, severe dry eyes, iritis or scleritis are each associated with ocular irritation and photosensitivity. This may lead to an increased blink rate or in some cases, excess squeezing of the eyelid muscles (“blepharospasm”). “Benign Essential Blepharospasm (BEB)” however, is a rare condition in which there is involuntary blinking of the eyelids as well as episodes of eyelid closure (spasms) that may be forceful and sustained (5-10 seconds). In contrast to the patient with a corneal foreign body where the cause of the excess blinking is known, the cause of Benign Essential Blepharospasm is unknown. The episodes of excess blinking and eyelid spasms are completely uncontrollable (Figure 1a and 1b). Benign Essential Blepharospasm is a type of Dystonia: a term used to describe abnormal, involuntary, sustained muscle contractions and spasms involving various parts of the body (e.g., torticollis, writers cramp, etc.).

Figure 1a – BEB patient – eyes are open.

Figure 1b – BEB patient with episode of eyelid spasms.
Benign Essential Blepharospasm most commonly affects individuals over the age of 50, with females more commonly affected than males. The eyelid blinking and spasms occur bilaterally. BEB usually begins with an increased blink rate and with time, progresses to episode of forceful eyelid closure (spasms) that may last for 5 to 15 seconds, occurring frequently through out the day. The eyelid spasms in BEB are unpredictable and occur at any time throughout the day. At times the patient may appear to have normal eyelid movement whereas, at other times the patient develops excess blinking and spasms with forceful eyelid closure. Many individuals report that bright lights, stress, fatigue, watching television and driving make the spasms worse whereas the intensity of squeezing is relieved by sleep and relaxation. Some patients discover maneuvers such as touching the eyelids, chewing, talking, humming, coughing or rubbing the forehead may allow temporary suppression of the involuntary squeezing.
Some BEB patients will develop other facial spasms such as lip pursing, chin thrusting and various tongue movements. Blepharospasm with areas of lower facial spasm is referred to as the “Miege Syndrome”.
To compound matters further, about 7% of patients with BEB also develop “Apraxia of eyelid opening” .Apraxia of eyelid opening refers to an inability to initiate the act of opening the eyelids, and usually follows an episode of eyelid spasm. It is not associated with contraction of the closing muscles of the eyelids, but rather an inability to activate the opening muscles. The eyelids simply remain closed after an episode of eyelid spasm and the patient is unable to open them for several seconds.
Treatment of Benign Essential Blepharospasm involves:
1) educating the patient about the disease
2) putting the patient in touch with a support group
3) oral medication ( of limited benefit in 5 – 10%)
4) botulinum toxin (extremely helpful)
5) myectomy surgery (primarily used for botox failures or inadequate response to botulinum toxin)
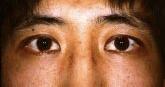
Hemifacial Spasm
Hemifacial Spasm (HFS), like the name implies, is characterized by an uncontrollable twitching of the muscles on one half of the face (Figure 2a and 2b) in contrast to Essential Blepharospasm which involves eyelid spasms bilaterally. Hemifacial spasm is most common in middle age (50’s, 60’s) but can begin at any age. Like Benign Essential Blepharospasm, it is more common in females. HFS usually starts as a mild twitching of the eyelid muscles, most commonly of the lower eyelid. It gradually spreads to involve the upper eyelid and then in time spreads over the face and neck on the same side. The twitches start spontaneously or may be precipitated by talking, tension, or fatigue. It is at first intermittent, but becomes more frequent and more severe as time passes. With time, the patient may develop prolonged contractions of the muscles, closing the eyelids and pulling the corner of the mouth toward the ear. Once prolonged contractions occur, there is often some facial weakness noted as well.

Figure 2a – Normal eyes.
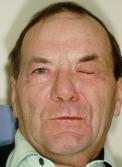
Figure 2a Notice the left side of the face in spasm.
In Hemifacial Spasm, there is an irritation of the 7th nerve in the brainstem. The commonest cause is a blood vessel pulsating against the facial nerve. Rarely, it is due to a tumor pressing on the nerve. All Hemifacial Spasm patients therefore require neuro-imaging such as a CT scan or MRI scan.
Treatment of HFS in the early phase is occasionally improved with oral medication such as a muscle relaxant. The most effective, but temporary improvement comes with botulinum toxin injections. The most definitive treatment involves neurosurgery to place a Teflon sponge between the artery and seventh nerve. This micro-vascular decompression is referred to as the “Janetta” procedure. While the surgery is generally successful, it is a neurosurgical procedure with the potential for serious complications (meningitis, stroke, permanent facial paralysis, permanent hearing deficit, post-operative blood clots and even death {rare}). Complete cure for HFS occurs in 80% of patients, 10% have marked improved and 10% do not improve.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.
The BOTOX® Craze
Commonly Asked Questions
INTRODUCTION
Despite recent marketing hype, BOTOX® (Botulinum Toxin A) is neither new, nor a cure all. BOTOX® was developed more than 20 years ago by an eye doctor to treat crossed eyes and muscle spasms around the eye. Although in my practice I have used BOTOX® since 1985 for eyelid spasms (Blepharospasm, Hemifacial spasm), wrinkles and frown lines, many physicians have just recently “discovered” it’s many benefits. The list of conditions it has been found to benefit seems to be growing almost on a monthly basis.
BOTOX® has become one of the most popular methods for treating frown lines and laugh lines in the eyebrow, forehead and eyelid area. The quick, painless treatment has no down time for healing, and produces marked improvement in wrinkles caused by dynamic contraction of facial muscles.
Exactly What is BOTOX®?
BOTOX® is the trade name for a neuro-toxin produced by a bacteria known as Clostridium. This bacteria is found worldwide in earth and water. Under certain low oxygen conditions, it activates and produces a protein called “botulinum toxin”. Such is the case when vegetable or meat products are contaminated by the bacteria and stored in an airtight container. If this contaminated food is ingested along with enough botulinum toxin, paralysis of various muscles throughout the body develops. This type of food poisoning is referred to as “botulism”. A purified version of the toxin in minute quantities (up to 500 times less than what would be needed to cause systemic symptoms) can weaken muscles when injected selectively into certain parts of the face.
How Does It Work?
When used in very small doses, BOTOX® works by paralyzing the muscles that create frown lines, crow’s feet, and horizontal forehead wrinkles. BOTOX® protein acts by preventing the release of a neurotransmitter (acetylcholine) at the nerve-muscle junction. Without acetylcholine the nerve cannot stimulate muscle contraction, and the overlying skin will therefore not wrinkle or fold. The result: smoothing of the overlying skin that lasts three to six months.
What Are The Side Effects?
It is very important to place the right amount of BOTOX® in the right place. The side effects of BOTOX® therapy are mild and self-limited and are more related to technique than toxicity. Occasionally a person may have some mild bruising or temporary swelling at the injection site. In less than 3% of patients, the upper eyelid may droop slightly, but this resolves as the drug is absorbed over the next few weeks. If a droopy eyelid does occur, an eye drop (Iopidine) is available to raise it. Having injected over 10,000 patients in the last 17 years, I am amazed at the low incidence of side effects with this product.
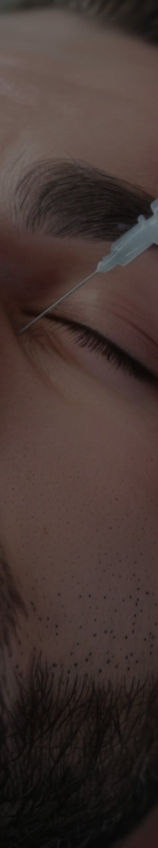
How Is The Treatment Performed?
BOTOX® is administered through a small acupuncture-sized needle at those sites requiring wrinkle reduction. The crows feet usually require 3 to 6 injection sites per side while the forehead may require 9-12 injections (depending upon the number of lines) and the wrink les between the eyebrows 6-7 injections. Although discomfort is minimal, topical anesthetic cream can be applied prior to the injection for those patients desiring it.
How Long Does BOTOX® Last?
Within 3 to 5 days of injection, the BOTOX® has taken effect to weaken the muscles. The human body slowly breaks down the botulinum protein until it is inactive and normal muscle function returns. Facial lines stay smooth for 3 to 6 months before another round of injections is needed.
Does BOTOX® Work In Everybody?
Almost everybody. On very rare occasions someone will have little or no response to the treatment. The lack of response is more likely due to in-adequate amounts of BOTOX® given, or BOTOX® administered in the wrong place due to lack of experience with the product. As a result the patient is unhappy and thinks the BOTOX® did not work. It is very important to place the right amount of BOTOX® in the right place. Following the first injection of BOTOX® the patient should be seen in follow-up about 2 weeks later to be sure the dose given was the right amount for that particular patient. Some patients do require more than others. The Botox injection (dose and injection sites) should be customized for each patient.
What If I Want To Keep Some Facial Expressions?
Too much BOTOX® will give the person a mask-like face. It is important to individualize BOTOX® treatments and find out exactly what each individual would like. This can easily be done. Having some facial expression is important, as it is essential for communication. When properly injected, BOTOX® will smooth frown lines, crows feet, furrowed brows and lines brought on by years of repetitive facial expressions.
Once I Start, Am I Committed To Using It?
No. You can try it, if you like it, have another when it wears off. If you want to wait for whatever reason, it’s okay to wait. Have another when you are ready.
What Are The Common Facial Areas That Can Be Treated With BOTOX®?
- Vertical frown lines between the eyebrows
- Horizontal forehead lines
- Crows feet
- Unequal brow height
- Upper lip wrinkling
- Down turning of the mouth
- Bunny lines along the side of the nose
- Horizontal neck lines
- Vertical bands in the neck
- VerticalOther: excess underarm sweating, hand or foot sweating
Does BOTOX® In One Area Cause Wrinkling In Adjacent Areas?
Generally not. When one area (ex. furrows between the brows) is treated, this area flattens out and becomes wrinkle free. Some patients will notice wrinkles in adjacent areas only because the area treated is so smooth. Thus, the wrinkles in other areas were actually there all along, it’s just that the patient is noticing them. Very occasionally, when a patient is trying to recreate a certain facial expression in an area with BOTOX® on board, the adjacent areas may seem to fold more, in an attempt to make the lost expression. This situation could potentially cause more noticeable wrinkling in adjacent areas. This can easily be treated by slightly broadening the area of BOTOX® injection so these adjacent muscles are also included in the BOTOX® treatment as well.
What About BOTOX® Parties?
BOTOX® parties are frowned upon by most physicians.
BOTOX® treatment should be customized to each patient’s desire and pattern of facial expression. The areas of injection should be discussed in a professional manner in an office setting with no outside influences acting. This is difficult to do in a social gathering where friends may be pressuring one another. Alcohol and BOTOX® do not mix. Alcohol is a vasodilator. Injecting BOTOX® into a patient with alcohol on board is potentially dangerous. With dilated vessels in the area of injection there is a greater risk for systemic absorption as well as an injection directly into the dilated vessels. Obtaining informed consent when the patient has alcohol on board invalidates the consent.
BOTOX® is a powerful drug that should be administered with care and with the appropriate Doctor-patient relationship respected. A party atmosphere with socialization of the Doctor and patient violates the ethical responsibility of the physician.
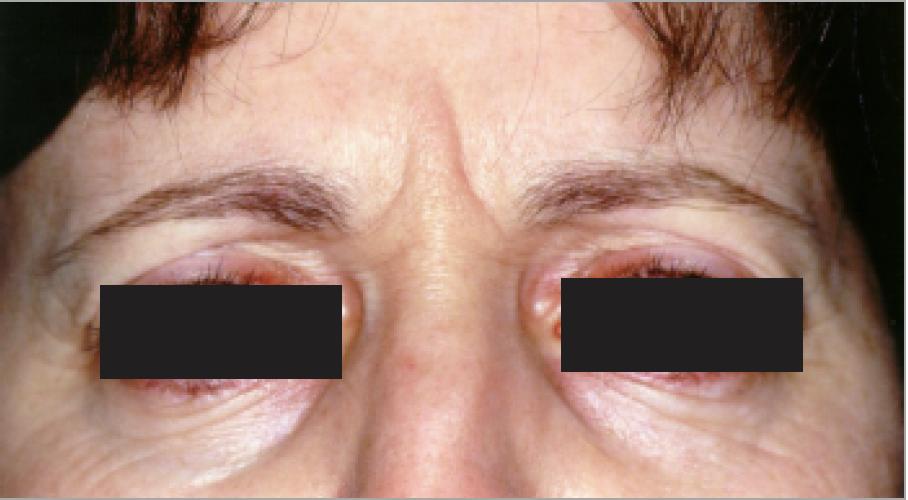
Figure 1
Pre Botox injection – lots of vertical frown lines.
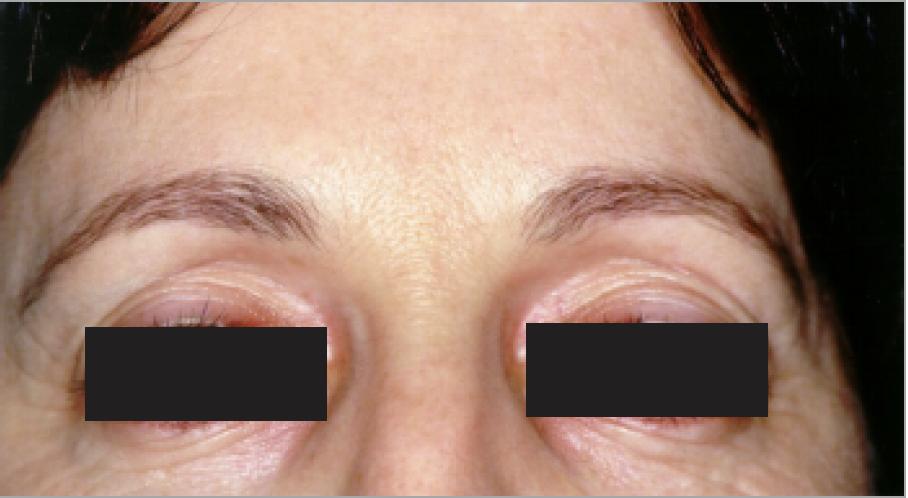
Figure 2
1 week post Botox injection – in the relaxed position → there are no vertical frown lines.
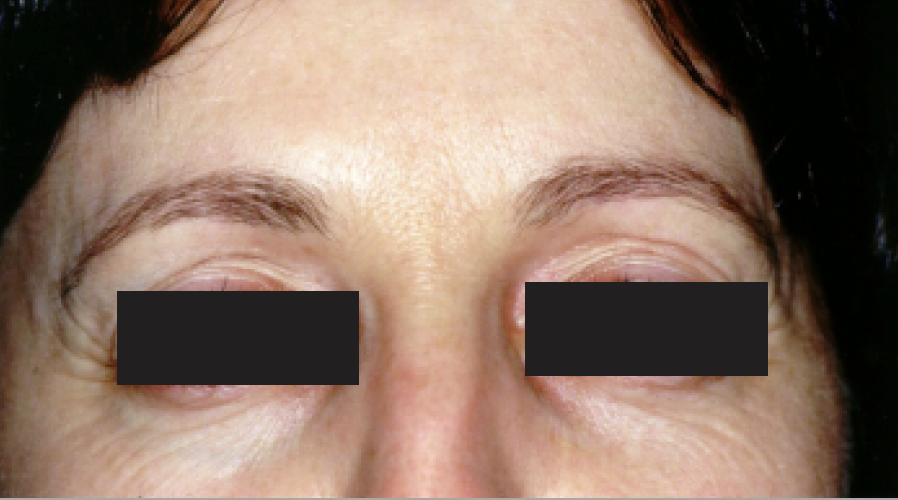
Figure 3
1 week post Botox injection – Patient is trying to frown but cannot. There are no vertical lines.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.
Cosmetic Eyelid Surgery
Commonly Asked Questions
INTRODUCTION
Your eyes are generally the first thing people notice about your face and are an important aspect of facial attractiveness. People with heavy or droopy eyelids are often perceived as being older than their age, tired, and of lower IQ than people with normal appearing eyelids.
The upper and/or lower eyelids become “droopy” or “baggy” over time as the eyelid skin stretches, muscles weaken and fat pockets bulge to become more prominent. This process most commonly occurs because of the aging process but also may be a hereditary condition that runs in ones family. Your eyebrows may also sag or droop as part of the same process.
As the excess skin and/or fat accumulates, the overall attractiveness of one’s eyes decrease leading to a tired and older appearance. When severe, these conditions may lead to an impaired field of vision (baggy upper eyelids) or difficulty wearing glasses (baggy lower lids).
When Should You Consider Cosmetic Eyelid Surgery?
Cosmetic eyelid surgery is a personal decision. Whenever you feel the excess lid skin and fat bags are affecting your facial attractiveness and the way you feel about yourself, it’s time to think about cosmetic eyelid surgery. Most people don’t start thinking about it until their forties, or fifties but it can be considered earlier or later depending upon the individual. From an anatomical standpoint as long as there is enough excess skin and fat to remove, make a visible difference, and, allow the eyelids to open and close properly, cosmetic eyelid surgery can be performed. The best time to do it is when the patient is motivated to have it done. It is an individual choice and each individual needs to make his/her own mind up with no outside pressure to do so.
What Are The Possibilities?
Upper Eyelids – in a surgical procedure known as blepharoplasty, incisions are made in the natural fold of the eyelids to remove excess skin, muscle or fat. Those incisions are then closed with very fine sutures so that, after healing, the surgical sites become virtually unnoticeable. This procedure relieves eyelid heaviness and unnecessary folds, leaving a smooth platform for makeup and a more youthful, energetic appearance.
Lower Lids – Blepharoplasty is also used to correct bulges or puffiness associated with the lower eyelids. Here, the incisions are made directly below the eyelashes to remove excess skin. If only fat and no skin needs to be removed, the incisions can be made behind the lower eyelids in a procedure known as transconjunctival blepharoplasty.
When Should The Brows Be Considered?
Male brows generally lay along the orbital rim or slightly lower while female brows generally are above the orbital rim or parallel to it. Once a female brow falls below the rim and a man’s well below the rim – brow elevation should be considered. If brow elevation is required but only the lids are done, the brows, postoperatively, may be pulled further downward into the lid. Many patients with low brows use their forehead muscles to keep the brows slightly elevated. Once the eyelid skin is removed the forehead muscles relax allowing the brows to fall. Some patients may complain following their upper eyelid surgery that there is little improvement post-operatively. What has actually happened is the eyebrows have fallen giving rise to a heavy eyelid appearance.
Is The Eyelid Surgery Covered By Health Insurance?
Health plans such as the Ministry of Health (OHIP) will only cover the eyelid skin removal on the upper lids if there is a 50% visual field restriction. The eyelid skin has to be covering the top of the pupil. Many people don’t get to this stage until their 70’s or 80’s. OHIP does not cover it simply because “it bothers you”, “you can see it in your field of vision”, or “it acts like a weight on the lid”. There must be a 50% visual field reduction for OHIP to cover it. OHIP will never cover eyebrow surgery even though the eyebrows are extremely low and may be contributing to a 50% visual field restriction.
What Is Involved In The Surgery?
Upper eyelid surgery is generally done under local anesthesia. The anesthesia is injected into the loose skin of the eyelid. Once frozen the excess lid skin ± fat is carefully removed. The incision is closed. The upper lids generally take 15 to 20 minutes per lid and it is not a painful procedure. The eyes are safe during the surgery.
Lower lids are slightly more involved and consume more time (average 1 to 1½ hours). The lower lids may be done under local anesthesia like the upper lids or may occasionally require intravenous sedation for nervous individuals. The eyes are safe during the procedure. Like the upper eyelids, the lower eyelid surgery is not painful.
What Is The Postop Care Routine And How Much Time Is Required Off Work Afterwards?
For upper and lower lids, rest with cool compresses placed over the eyelids every 3 to 4 hours are required to help with bruising and swelling in the first 3 days. In between these times the patient can be up but taking it easy. Thereafter, one can go out but should wear sunglasses as the lids will appear puffy and bruised. If one is too active in the first few days, bleeding could be stimulated which will prolong the recover and could have potential side effects to the eye. I generally recommend 1 week away from work or social gatherings when upper lids are done and 2 weeks when lower lids are done.
Is Cosmetic Eyelid Surgery Safe?
With any surgery there are risks and complications. If the surgery is being performed by an experienced individual preferably with a subspecialty in eyelid surgery, the chances of problems lessen significantly.
Anytime there is an incision in the skin there is a risk of infection. The risk is extremely small. Similarly, anytime there is a cut in the skin there is a risk of bleeding or bruising. This risk can be significantly decreased by avoiding Aspirin, blood thinners, anti-inflammatory medications,
Vitamin E, Ginko Biloba, etc. in the week before surgery as well as resting postoperatively with cool compresses over the lids. If bleeding occurs postoperatively for whatever reason and builds up in the eyelid, it may cause unsightly swelling, pain and potentially apply pressure to the eye which may then affect the vision if not attended to. Following postoperative instructions for rest and the use of cool compresses is extremely important. Scarring is uncommon and can be reduced by meticulous surgical techniques as well as careful post-op care with Vitamin E oil, topical steroid cream and silicone gel to the incision line. In most instances the upper lid incisions blends into the eyelid crease, while the lower lid incision hides just below the lashes. Slight asymmetry of the eyelids may occur if uneven amounts of skin are removed. This can be corrected easily with a small touch up performed generally at 3-4 months post-op. Vision should not be affected other than some mild blurring of vision post-operatively when ointment is being applied to the eyelid incision area and may get into the eye. Rarely, a change in glasses or contact lenses is required post eyelid surgery.
How Does One Avoid The “Wind Swept or Surprised Appearance”?
The best answer I can give is to have your eyelid surgery done by an experienced physician well trained in the eyelid area. In this day and age, there are many types of surgeons performing eyelid surgery including Ophthalmologists (Eye Doctors), Otolaryngologisrts (Ear/Nose/Throat surgeons), Plastic surgeons, General Practitioners, General surgeons, etc. Their training, however, is not the same. An Ophthalmologist with 1-2 additional years of subspecialty training in the eyelids is referred to as an Ophthalmic Plastic and Reconstructive Surgeon or an Oculoplastic Surgeon. An individual with training in this area generally does more eyelid surgery and has more knowledge of the eyelid anatomy than any of the other group of physicians doing this. Although this does not guarantee a lack of complications, it decreases the chance. Furthermore, Ophthalmologists are the only ones qualified to take care of the eye should the patient experience eye troubles following the eyelid surgery. It makes sense to have cosmetic eyelid surgery performed by the individual most qualified to not only do the eyelid surgery, but, also take care of the eye should any eye problems arise.
What Should You Look For In An Eyelid Surgeon?
A qualified individual who has many years of experience and who individualizes his eyelid surgery technique for each patient. Eyelids are not all the same and the surgeon that treats them this way is first one to avoid. Some people need skin removed, others skin and fat, others require brow elevation as well as skin and fat. Removing fat in lids that don’t actually require it will leave the eyelid area with a hollow appearance. Caucasian eyelids are different from Asian eyelids. If the Asian eyelid is treated like a Caucasian eyelid, the Asian patient develops a very unnatural appearance.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.
Cosmetic Enhancement in the Eyelid Area
Considerations and Possibilities
INTRODUCTION
As one ages, the upper and lower lid skin stretches, muscles weaken and fat pockets bulge. Aesthetically, such conditions may detract from the overall attractiveness of ones eyes and cause a “tired” or “older” appearance. This situation bothers some individuals more than others, and at different ages. There are a number of ways one can improve the appearance of the eye area, including surgical as well as non-surgical options.
What Are The Possibilities?
- Upper Eyelids – In a surgical procedure known as blepharoplasty, incisions are made in the natural fold of the eyelids to remove excess skin, muscle or fat. These incisions are then closed with very fine sutures so that, after healing, the surgical sites become virtually unnoticeable. This procedure relieves eyelid heaviness and unnecessary folds, leaving a smooth platform for makeup and a more youthful, energetic appearance.
- Lower Eyelids – blepharoplasty is also used to correct bulges, puffiness and wrinkles associated with the lower eyelids. Here the incisions are made directly below the eyelashes to remove excess skin. If only fat and no skin needs to be removed, the incisions can be made just behind the lower eyelids in a procedure known as transconjunctival blepharoplasty.
- Forehead Frown Lines – Vertical lines in the mid-forehead, usually called “frown lines”, can be eliminated or minimized through injection of minute quantities Botox™. Horizontal lines running across the forehead can also be treated in a similar fashion. Botox™ temporarily weakens the over-acting muscles that create these wrinkle lines for 3-9 months. A soft tissue filler such as Restylane is also beneficial to reduce the unwanted verticial lines between the eyebrows.
- Eyebrows – Droopy brows may be elevated through a procedure known as an eyebrow or forehead lift. Small incisions are made directly above the eyebrows or within the forehead creases. In a coronal brow lift, the incision is made at or just behind the hairline. In the endoscopic technique, several small incisions are placed in the scalp and the entire forehead is lifted using an endoscope. Botox™ may also be used to raise the eyebrows in selected patients.
- Sun Damage – The first step to treat photo damaged (sun damaged) skin is to stop the ongoing photo damage. It makes little sense to spend a lot of time and money to improve the quality of skin and then subject it to further damage from chronic ultraviolet (UV) light exposure. Your skin has the ability to repair itself if it is protected from continual damage. A sun blocker that protects from UVA (causes most of the aging and wrinkle changes) and UVB (causes skin cancer) is most beneficial. Most sun blocks have a rating for UVB protection but lack a rating for UVA protection. Study the label carefully or ask the pharmacist if there is UVA protection.
Skin damaged by the sun can be treated through the use of rejuvenative creams and lotions that minimize pigment spots and naturally thicken the skin to provide a more healthy and youthful appearance. A sun block started at any time in one’s life will help prevent further solar damage.
Cosmetic Eyelid Surgery – Should I Do It?
Removal of the excess skin and fat can restore a younger, more rested appearance but the surgery required is an individual decision. Patients should research the procedure through reading, internet, friends who have had it, as well as through consultation with a physician experienced in the field. It is important to then take some time and think over the advantages and disadvantages, risks, etc. The best time to consider cosmetic eyelid surgery is when the patient is truly ready and motivated to do it. It’s not a good idea if one is not sure, stressed out, going through a separation/divorce, or, experiencing another major life change. One shouldn’t feel outside pressure to have it.
Patient Expectations
Cosmetic eyelid surgery can remove some of the excess skin and fat and restore a more youthful and rested look. However, only so much tissue can be removed. It is important to leave enough skin behind to balance the rest of the face and most importantly allow proper eyelid closure. If the eyelids don’t close properly, eye irritation may occur which can be quite bothersome and lead to discomfort, tearing, photosensitivity, etc.
Choosing The Right Surgeon?
Eyelids are not the same. They are slightly different from person to person, race to race. One patient’s eyelids may require fat repositioning, while another patient may need fat resection, and a third may be in need of a special tightening effect of the lower eyelid. It is important to individualize the treatment plan for each particular patient’s needs.
Performing surgery in the area surrounding the eye requires a delicate hand, an artist’s vision and most importantly, extensive knowledge and specialized training. If you intend to see one or more surgeons before choosing one, there are questions you can ask to compare them. Examples:
What formal training have you had in cosmetic eyelid surgery
- A weekend course, a few cases as a resident?
- A formal, credentialed fellowship (usually 1 or 2 additional years), or other extended, advanced training in this area?
- A How long have you been performing cosmetic eyelid surgery?
- Are you credentialed by any recognized national organization?
- What are the complications of cosmetic eyelid surgery and are you trained to handle them or will you have to refer such complications to other physicians?
- If you need to refer, to whom do you send your patients?
For your information, Dr. Jordan served two additional years of fellowship training in Ophthalmic Plastic and Reconstructive Surgery with leading experts in the world in 1986 and 1987. This was after having fulfilled four years of medical school, a one-year internship and 3 years of residency training in Ophthalmology. Dr. Jordan has been performing cosmetic and reconstructive surgery in the eye region exclusively since 1986. He is credentiated by and is an active member of the American Society of Ophthalmic Plastic and Reconstructive Surgeons (ASOPRS) and is the only physician in the Ottawa area credentialed by this group.
Dr. Jordan will discuss with you all possible complications of your surgery. He is fully qualified to deal with any complications dealing with the eye or eyelid. Other surgeons routinely refer their eyelid complication cases to Dr. Jordan for management.
Tips For Successful Outcome:
1) Choose your surgeon carefully. Be sure he/she has lots of experience. Ideally they should have an additional training in the field of Ophthalmic Plastic and Reconstructive Surgery.
2) Review your concerns carefully with the surgeon and be sure the surgeon plans to individualize the surgery to your anatomy (i.e. not all eyelids are the same).
3) Follow post-op instructions carefully – give your body a chance to heal. Rest with ice packs in the first 48 hours is most important. If you are too active in the first few days, you may upset the healing process.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.
Blepharoplasty
For Functional and Cosmetic Indications
INTRODUCTION
Having eyelid surgery to remove excess skin and fat is referred to as a “Blepharoplasty”. Motivation for this type of procedure may be either functional or cosmetic.
Functional blepharoplasty
As one ages, the upper and lower lid tissues begin to relax. These nonspecific changes may be accelerated by sun exposure, allergies or recurrent swelling and consist of stretching or senile elastosis of the skin. In some individuals, this process may be hereditary. The result is an excess of eyelid tissue referred to as “dermatochalasis”. Stretching and relaxation of the orbital septum will allow prolapse of the orbital fat into the eyelids. As a result, a “fullness” to the lid develops which increases over time. This excess lid tissue creates a tired look, may cause the patient to look older than they actually are, and may cause a heavy feeling or weight on the lid. With time, the excess lid tissues in the upper lid may hang over the lid margin and cause a visual field restriction. Patients may describe it as “something sitting there”, “like wearing a baseball cap”, or “like a shadow at the side”. In the lower lid, the excess skin and fat do not cause as much of a problem but can occasionally affect the bifocal portion of the glasses. Patients with excess skin in the upper lids causing a visual field restriction or in the lower lid affecting the bifocal segment have a functional defect that can be alleviated by surgical removal of the skin, and fat, leading to an improved and more comfortable field of view.


Top figure – 48 year old female pre-op.
Bottom figure – Post 4 lid blepharoplasty.


Top figure – 70 year old male pre-op.
Bottom figure – Post 4 lid blepharoplasty
Cosmetic blepharoplasty
Your eyes are often the first thing people notice about your face and are an important aspect of facial attractiveness. Unfortunately, with age, the upper and lower eyelids become “droopy” or “baggy” in appearance. Aesthetically, such conditions may detract from the overall attractiveness of ones eyes and cause a “tired” or “older” appearance. This situation bothers some individuals more than others (female > male) and at different ages. Removal of the excess skin and fat can restore a younger, more rested appearance.
Preoperative consideration
A preoperative ophthalmologic examination is essential, to document the visual acuity, baseline tear function, tear film stability, strength of lid closure, symmetry of palpebral aperatures, previous lid incisions, etc. The pre-existence of dry eyes, residual facial palsy, lid closure problems from previous surgery or ptosis will have a definite bearing on the extent of the lid surgery.
For those considering surgery for functional reasons, a visual field test is required. If the visual field shows a reduced peripheral field of view, the surgery may be covered by OHIP. Preoperative photos may also be required for preauthorization.
In the cosmetic patient, it is essential to establish what they find bothersome in their appearance and what they expect surgery to accomplish. This process can be aided by handing the patient a mirror and asking them to point out what they would like corrected. Patients may point out skin discoloration, deep creases, cheek fullness and other features that may not be correctable by eyelid surgery alone.
Blepharoplasty is able to remove the bulges created by fat herniation and excess skin that is becoming redundant. Patients need to know they have to have some skin available to allow proper eyelid opening and closing. Enough skin has to remain to allow this. Many patients want “all” the fine lines removed on their lids (especially lower lids and crows feet). With skin removal by scalpel, the fine lines will diminish in their appearance but to remove them all, may prevent normal eyelid closure. Laser skin resurfacing is more effective in removing the fine lines than scalpel but even with laser it may not be possible to remove all of them. This is especially so in the crows feet area which may display a lot of wrinkling, especially with facial expression.
The goal of surgery is to remove excess wrinkles and fat. The patients look more alert and healthy, less tired and generally have a younger, more rested appearance. Surgery should allow the eyelids to open and close properly without any distortion or change in the natural almond-shaped lid contour and, with incisions that remain hidden.


Top figure – 45 year old female pre-op.
Bottom figure – Post 4 lid blepharoplasty
Top figure – 35 year old oriental male pre-op.
Bottom figure – Post upper lid blepharoplasty with re-creation of Caucasian lid fold.
Surgery
Many different specialists (of varying qualifications) perform this type of surgery including Ophthalmologists, Plastic Surgeons, Otolaryngologists and Dermatologists. Cosmetic (and functional) eyelid surgery is commonly performed by Ophthalmic Plastic and Reconstructive Surgeons who are Ophthalmologists that have completed one or two additional years specializing in treatment of problems that involve the eyelids, lacrimal system, orbit and adjacent facial structures. The complications associated with Blepharoplasty are eye related. It makes sense to have the surgery done by someone who has a thorough knowledge of the eye and is able to manage those potential eye problems that occasionally occur.
Blepharoplasty surgery is an out-patient procedure performed under local anesthesia, with sedation if desired. During surgery, incisions are made in the natural folds of the eyelid so they are almost invisible after proper tissue healing.
If only fatty tissue needs to be removed from the lower lids and not any skin, the surgery can be performed from behind the eyelid. This is known as “transconjunctival blepharoplasty”.
In cases where the eyebrows are also droopy, a procedure to elevate the eyebrow may be appropriate. This procedure, known as a “brow lift”, may be done directly above the eyebrow within the forehead creases or by an endoscopic approach.
After surgery
Following surgery, cold compresses for 3 to 4 days and antibiotic ointment, followed by warm compresses are used to help the healing process. Eye patches are not required. Discomfort is usually minimal and handled by acetaminophen. Aspirin containing compounds should be avoided because of their tendency to increase bruising. Most individuals will have swelling and some degree of bruising that will settle over the first 1 to 3 weeks. Patient healing however, is variable with some healing much quicker than others. Complete tissue healing usually occurs by 2 to 3 months. For upper lid blepharoplasty, one week off work is average while 2 weeks is best in those having 4 lid blepharoplasty. Makeup can be applied to help hide residual bruising after one week.
Complications
After surgery, the patient may temporarily experience minor discomfort, tightening or numbness of the lids, swelling, bruising and dryness of the eyes. The eyelid blink rate temporarily slows down after the surgery and, as a result, the eyes may have a gritty or sandy feeling. Artificial tears during the day and lubricating ointment at night are commonly used to keep the eyes moist during the healing process. As the incisions heal and the eyelid mobility returns to normal, these symptoms will usually resolve. Excessive pain, bleeding, and infection are very uncommon. Blurry vision may occur during the healing period as a result of the decrease in eyelid blink rate or ointment getting into the eye but should return to normal in one to two weeks. Loss of vision has been reported following this surgery but fortunately is extremely rare and very few blepharoplasty surgeons will ever encounter it. The exact incidence is unknown but is probably in the order of 1 in 2,500, (0.04%). The cause is usually deep orbital hemorrhage likely secondary to excess traction on the fat.
Once the healing process has settled (average 2 to 3 months), if there is any lid asymmetry, a touchup procedure may be required in less than 5% of patients.
SCALPEL vs. LASER
Both have advantages and disadvantages. In general, for the upper lids, there is really not much difference in the end result as the same amount of skin is being removed. For the lower lids if there is a lot of redundant skin, scalpel is beneficial. If there are mainly fine lines, laser is more effective. Laser on the lower lids may however, have a longer recovery period, depending on the skin type and laser used.
SUMMARY
Blepharoplasty surgery can provide both functional and cosmetic improvement with minimal risk of serious problems. Most patients are quite pleased with the results of their eyelid surgery.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.
Assessment of the Patient with Droopy Lids
INTRODUCTION
Droopy eyelids are common in the aging population and may involve one or both lids. What one physician refers to as a “droopy eyelid” how-ever, is not always what another is referring to. The drooping appearance may be due to: true “eyelid ptosis”(levator aponeurosis thinning or disinsertion), “excess eye-lid skin” (dermatochalasis),“brow ptosis”, “contralateral eyelid retraction”, “enophthalmos” (sunken eye) or, a combination of the above. The treatments for these various problems are different and it is essential to sort out which of the contributing factors are present in each individual so that an appropriate management plan can be organized
Eyelid Ptosis
Ptosis (pronounced “toe-sis”) of the eyelids refers to a drooping of the upper eyelid as a result of a problem with the eyelid elevating muscle (the levator). The lid droop may be minimal or it may droop to partially or completely cover the pupil and restrict the superior visual field [Figure 1].
Ptosis may be congenital or acquired. Congenital ptosis is present at birth and is commonly due to a dystrophic levator muscle while acquired ptosis develops with age. The commonest type of acquired ptosis is due to a thinning and/or disinsertion of the levator aponeurosis (that portion of the levator muscle which inserts onto tarsal plate). Other types of acquired ptosis are mechanical (due to a stye, chalazion or eyelid tumor), traumatic (blunt or surgical i.e. post cataract surgery), myogenic (i.e. myasthenia gravis), or neurogenic (i.e. Horners syndrome).
The treatment for eyelid ptosis (with the exception of myasthenia) involves an advancement of the levator aponeurosis onto the tarsal plate, with a resultant lifting of the eyelid.

Figure 1– True eyelid ptosis as a result of levator thinning. The eyelids are covering part of the pupil.
Excess Eyelid Skin (Dermatochalasis)
Excess eyelid skin that hangs over the eyelid margin also gives the eyelid a droopy appearance, but for a different reason than true eyelid ptosis. With dermatochalasis, it is the skin hanging over the lid margin that is responsible for the drooping appearance [Figure 2a]. The underlying eyelid height may be normal or low depending upon whether any true eyelid ptosis exists. The way to assess this situation is to gently raise the excess lid skin off the eyelid [Figure 2b] and measure the lid height either with a ruler or by shinning a light at the eye from a distance of 2 feet or so. A normal eyelid fissure height is generally about 10 mm. By shinning a pen light toward the patient from a two foot distance a light reflex is created on the cornea. The distance between the light reflex and the upper lid margin is termed the “margin to reflex distance” or MRD. The MRD is usually 4 mm. A value of 1 or 2 is abnormal and indicates a true ptosis of the eyelid is also present.

Figure 2–Excess eyelid skin responsible for drooping appearance of lids.

Figure 3– When the excess eyelid skin on the patient’s right upper lid is gently lifted, the true eyelid height is found to be at a normal level.
Treatment of dermatochalasis involves removal of excess skin and fat on the eyelid (blepharoplasty). The levator aponeurosis is not touched unless of course the patient has a true lid ptosis as well. In this latter situation the appropriate surgery would then involve a levator aponeurotic advancement in conjunction with removal of excess skin and fat (blepharoplasty).
Brow Ptosis
A man’s brow is generally more full, straighter and rests at level of the orbital rim, while a lady’s brow is thinner, curved and generally sits above the orbital rim.
As we age the fibrous connective tissue structures within our facial tissue becomes lax and as a result tissues begin to sag due to gravitational forces pulling downward. A gradual migration of the eyebrow inferiorly is a result of these aging changes. As the eyebrow moves downward the excess eyelid skin appears to be more than it actually is and gives rise to a droopy eyelid [Figure 3a]. This phenomenon can be assessed by finding where the brow is in relation to the orbital rim. If the aging male or female brow is sitting below the rim, gently elevating it to the rim level or slightly above will elevate some of the excess eyelid skin (that component contributed by the droopy brow) so that one can get an appreciation of the true excess eyelid skin and true eyelid height [Figure 3b].

Figure 3a– Severe brow ptosis giving a droopy appearance to lids. The brows are below the orbital rims.
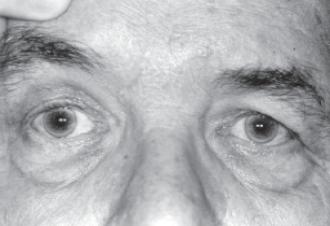
Figure 3b– When the patients right brow is elevated to a normal level, the true eyelid height is found to be normal and there is only a small degree of excess lid skin (dermatochalasis).
It is extremely important to sort out whether the brows are playing a role in the “droopy eyelid”. If the patient with brow ptosis and excess lid skin simply has the eyelid skin removed, the droopy eyelid may not be corrected as the brows will still be low and may appear to be sitting in the upper lid. In fact, the brow droop may even appear more noticeable following the eyelid skin removal since removal of the lid skin may pull the brow further downward (into the lid). Sometimes brow elevation on its own, by lifting the excess lid skin upwards, is all that is needed to correct the so called droopy eyelid. More commonly the patient with brow ptosis has a combination of brow ptosis and excess lid skin. In this case brow elevation on its own will only partially correct the excess lid skin, and a brow elevation with upper lid skin/fat removal (blepharoplasty) is more appropriate. It is also possible for the patient to have brow ptosis, dermatochalasis and true lid ptosis all at once. In this situation the patient requires brow elevation, blepharoplasty, and levator advancement surgery. Simply doing one will not correct the others.
Brow elevation surgery can either be done immediately above the brow hairline, in the mid-forehead, along the temporal hairline or endoscopically behind the frontal hairline, depending upon the patient’s facial features.
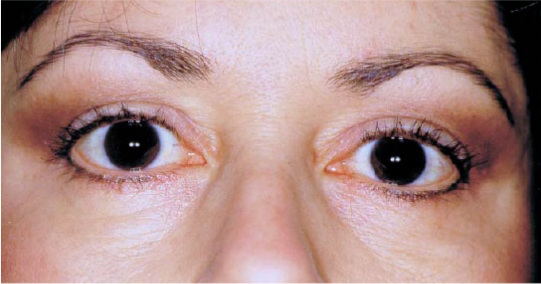
Contralateral Eyelid Retraction
Sometimes a patient presents with a drooping upper lid that actually has a retracted opposite upper eyelid. This situation is most commonly due to unrecognized Thyroid eye disease (Grave’s disease). The so-called droopy eyelid is only droopy in comparison to the opposite lid which is actually retracted superiorly. The lid retraction may be partially hidden by excess skin [Figure 4a] (dermatochalasis) and only becomes apparent if the lid skin is gently lifted [Figure 4b]. This type of patient requires a thyroid work-up including a medical history looking for systemic signs, family history of others with thyroid disease and a TSH test. If all are negative they need to be followed for several months as lid retraction is occasionally the initial sign of thyroid eye disease, despite a normal TSH test. Systemic hyperthyroidism may not show up for months or years later.

Figure 4a– Patient presented with ptosis of her right upper lid. It is actually the left upper lid that is too high (partially hidden by excess skin).

Figure 4b– The left upper lid retraction becomes more obvious as one gently lifts the skin on the left upper lid upward by manually elevating the left brow.
Enophthalmos and Droopy Eyelids
Enophthalmos refers to a sunkeness of the orbital tissue. It is not uncommonly seen following a blow to the orbit causing an orbital fracture. The fractured bones allow an increase in the orbital volume and as a result the eye moves posteriorly. As the eye moves posteriorly the upper lid may fall creating a droopy lid appearance.
The droopy lid appearance is a direct result of the expanded orbital volume. This situation is often referred to as a pseudo-ptosis (a false ptosis since the lid isn’t the problem).
To correct the false eyelid ptosis one needs to correct the enophthalmos. Correction of the enophthalmos requires restoration of the orbital volume. During floor fracture repair the orbital tissue that is herniated into the maxillary sinus, is repositioned into the orbit. A plate of some variety (supra-mid, Teflon, porous polyethylene, titanium mesh) is used to cover the bony defect, prevent re-herniation of the tissue and allow a restoration of the orbital volume.
Enophthalmos may have a more sinister problem associated with it. It is not uncommon for metastatic breast cancer to show up in the orbit 20 years later (even following appropriate treatment of the breast cancer), with a pseudo-ptosis as the result of enophthalmos. The matastatic breast cancer cells create a fibrosing reaction within the orbital tissue. As a result the eye is pulled posteriorly (enophthalmos) and the eyelid falls giving the appearance of an eyelid ptosis [Figure 5].

Figure 5b– Patient has a ptosis involving her right upper lid as a result of a metastatic tumor in the right orbit pulling the eye back (enophthalmos).
Summary Examination of the patient with a “droopy eyelid” should involve an assessment of the:
1. Eyelid height (true ptosis and contralateral eyelid retraction)
2. Brow position
3. Eyelid skin (dermatochalasis)
4. Enophthalmos
Appropriate treatment can only be performed if the surgeon knows the contributing factors and corrects them.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.
Tearing in Adults
INTRODUCTION
The lacrimal gland, located under the upper eyelid along and posterior to the lateral orbital rim is responsible for the production of tears. The gland produces a baseline amount of tears to moisten the cornea and will also respond to emotion or eye irritation by producing larger quantities of tears.
The nasolacrimal system is located medially and responsible for tear drainage. Each eyelid has a punctal opening and canaliculus which drains tears into the nasolacrimal sac and then into the nose [Fig. 1].
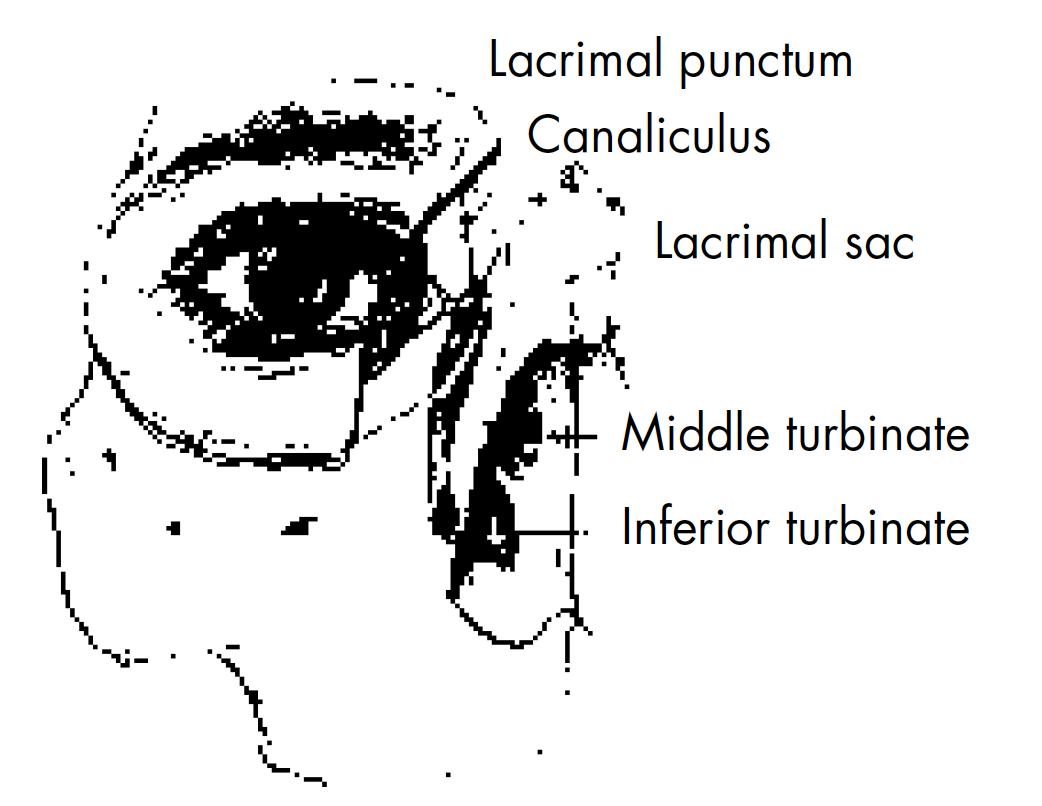
Figure 1 – Nasolacrimal system anatomy.
Tears may well up in the eye because too many tears are produced or because the tears are not being drained properly. Excess tears from any cause give the eye a moist appearance. Increased tear accumulation can also cause difficulty with reading. Tears continually running onto the cheek are annoying and may cause skin irritation from the regular wiping that results.
What causes excess tearing in adults?
Injury, birth defects, narrowing of the nasolacrimal system associated with age, eyelid malpositions, and infection, especially of the lacrimal sac, can lead to improper tear drainage at the punctum, canaliculus, lacrimal sac or nasolacrimal duct and lead to a back-up of tears which then overflow on to the face.
Eye infections, inturned eyelashes, exposure to the wind, yawning, glaucoma, certain drugs, eye strain or even Dry Eyes can also cause excessive tearing, by an increase in the amount of tears produced.
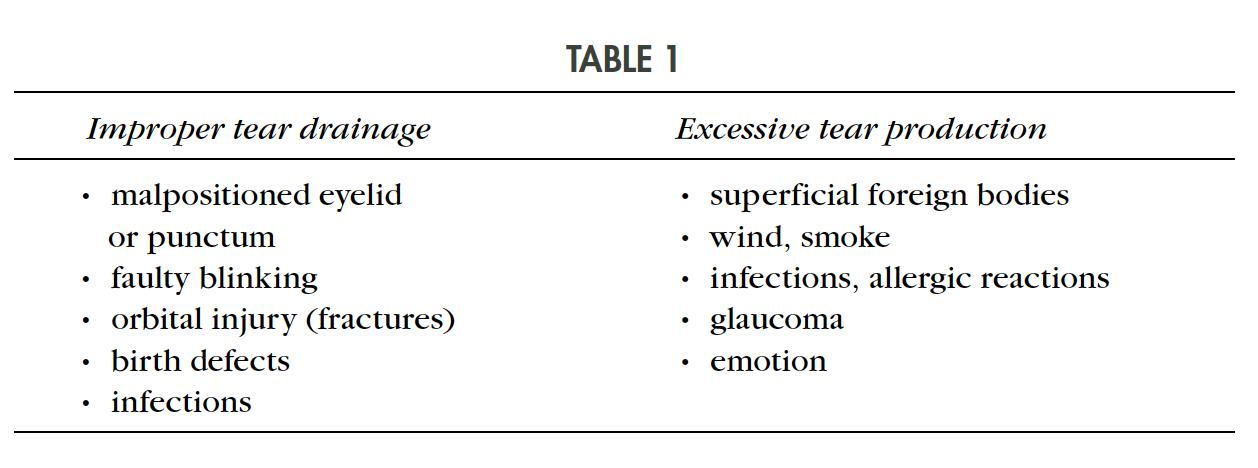
When a patient presents with tearing, it is important to determine whether there is excess tear production or improper tear drainage (Table 1).
How does one determine a cause for the tearing?
The eyelids need to be in normal position and have a good tone in order for the tears to be exchanged over the cornea and pumped into the tear canal.
Excessive tearing does not always mean an excess of tear production or blockage of the drainage system. Patients with a dry eye, not uncommonly, present to the office complaining of tearing. When the amount of baseline lubricating tears secreted is too low to maintain necessary moisture for the eye, the lacrimal gland reacts by producing additional tears. The nasolacrimal system may not be able to handle this out pouring of additional tears which then leads to episodes of tears overflowing onto the face, even though the underlying problem is too few baseline tears. This is often referred to as “reflex tearing”. The patient may complain of burning eyes or dry, sandy eyes which is a tip off to the diagnosis. If they do not volunteer this information by history, they should always be asked about symptoms of dry eyes.
Sometimes there are obvious clues to the diagnosis of a tearing problem as one interviews the patient. Examples include, facial nerve paralysis, traumatic scars involving the lids, ectropion, entropion, excoriation of the lid skin (dermatitis), congenital developmental eyelid anomalies. Each of these conditions can either upset the normal blinking rate and lead to tearing or cause eye irritation which leads to an increase production of tears which “overflow” onto the face, e.g. lashes rubbing on the cornea in entropion.
Infection in the nasolacrimal sac (“Dacryocystitis”) is usually obvious and presents with redness, swelling, pain and discharge [Fig. 2].

Figure 2 – Dacryocystitis illustrated.
If there are no clues on history or eyelid examination, various tear studies are required. A Schirmer study measures the amount of baseline tear production and is a good test for detecting dry eyes. A dye disappearance test is useful to determine the physiologic patency of the nasolacrimal system. In this test, a drop of 2% fluorescein dye is placed into the conjunctival fornix and observed. It should disappear by 5 minutes. If it does not, there is some degree of holdup in the outflow tract. Irrigation of the nasolacrimal system can also be done to see if there is complete blockage or whether the system is simply narrow. Dacryocystography is a diagnostic test requiring injection of dye into the nasolacrimal system followed by an x-ray. This allows examination of the anatomy of the lacrimal system to determine if there is a stone [Fig. 3] or other obstruction causing the excessive tearing. Lacrimal scintillography involves placing a radionucleotide labelled eye drop into the conjunctival fornix, followed by a measurement of the rate at which it disappears into the rest of the system.
Figure 3 – Example of a nasolacrimal sac stone.
Very occasionally, the exact cause cannot be determined. In such cases, the patient may have to learn to live with the tearing problem.
How is excessive tearing treated?
Very occasionally, the exact cause cannot be determined. In such cases, the patient may have to learn to live with the tearing problem.
Treatment depends on the problem. If the patient is felt to have dry eyes, a trial of artificial tears is recommended. If this does not help, the punctal openings can be blocked with small plugs to allow more retention of tears. If tearing is secondary to irritation by an inturned lash, the lash is removed. This can be done manually at first. If the lash recurs, it can be ablated with cryotherapy, electrolysis or with laser. Abnormalities of the eyelid (entropion, ectropion) require simple reconstructive procedures done under local anesthesia. For facial paralysis, a tarsorrhaphy may be required.
If the nasolacrimal duct is severely narrowed or completely blocked, surgery to open it is required (Dacryocystorhinostomy). This procedure is done under local stand-by anesthesia (intravenous narcotic and anxiolytics). The nasolacrimal sac and surrounding tissues are frozen with local anaesthesia (2% xylocaine with epinephrine). The nasal passage is also frozen with medication such as cocaine which also leads to vasoconstriction of the tissues. During surgery, the nasolacrimal sac is opened and anostomosed to the nasal mucosa. A silicone tube is then placed in the nasolacrimal system and left for 6 to 10 months to maintain the passageway [Fig. 4]. Removal of the tube is carried out in the office simply by cutting the tube and letting it fall out.
Very occasionally, the nasolacrimal sac is totally scarred shut and cannot be opened. In these instances, a small pyrex glass tube (Jones tube) is put in place to drain tears from the eye into the nose [Fig. 5]. The tubes are generally well tolerated and serve as a conduit for tear passage. They occasionally need rinsing to keep them open and occasionally need to be exchanged, each of which are minor office adjustments.
What complications can occur with tear duct surgery?
95-97% of the Dacryocystorhinostomy surgeries work fine and the tearing resolves, whereas 3-5% will not work and the patient remains with a tearing problem. Complications postoperatively are generally of a minor nature. Swelling around the incision, and eyelids, maybe present postoperatively and settles with ice packs. The incision for this surgery sits at the junction of the nose and eyelid and blends into the surrounding tissue nicely. By 3 months, it is almost invisible in over 95% of patients. As with any surgical procedure, there is the possibility of infection but it is very uncommon.
What complications can occur with tear duct surgery?
95-97% of the Dacryocystorhinostomy surgeries work fine and the tearing resolves, whereas 3-5% will not work and the patient remains with a tearing problem. Complications postoperatively are generally of a minor nature. Swelling around the incision, and eyelids, maybe present postoperatively and settles with ice packs. The incision for this surgery sits at the junction of the nose and eyelid and blends into the surrounding tissue nicely. By 3 months, it is almost invisible in over 95% of patients. As with any surgical procedure, there is the possibility of infection but it is very uncommon.
Figure 4 – Example of a nasolacrimal sac stone.
Figure 5 – Jones tube illustrated.
Bleeding from the nose or surgical site occasionally occurs to a minor degree on the day of surgery and it is common to develop a black eye after this procedure. Continued and heavy bleeding resistant to manual compression of the nose is uncommon and may require a return to the hospital with placement of a nasal pack for 24 to 48 hours. The silicone tubes may cause some minor eye irritation for 1 to 2 weeks. They are very well tolerated for the 6 to 12 months that they are in place but occasionally may lead to a smell in the nose which, if persistent, will lead to early removal.
Occasionally the new tear duct passageway will scar shut (3-5% of cases). If this occurs, simply re-placing the tubes back into the passage for an additional 6 months may be all that is needed to re-open the system. At other times, a revision of the procedure may be suggested.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.
Dry Eyes
INTRODUCTION
The term dry eye, refers to a group of disorders of the tear film with a reduced tear production or excessive tear evaporation that are associated with symptoms of ocular discomfort and that may cause damage to the ocular surface.
The cornea is kept moist by the lubricating effect of tears which are exchanged regularly with each eyelid blink. Tears are produced by 2 methods. One method (basic tear secretion) produces tears at a slow, steady rate and is responsible for normal eye lubrication. The other method (reflex tear secretion) produces large quantities of tears in response to eye irritation (foreign body) or emotions such as crying. The tears themselves are made up of a delicate balance of oil, water, and mucous; produced by various glands in the eyelid and conjunctival area. Dry eyes may be caused by changes in the quantity and/or quality of the natural tears produced by the various tear forming glands (lacrimal gland, meibomian glands, goblet cells, glands of Krause, and glands of Wolfring).
What are the symptoms of a dry eye?
The usual symptoms and signs include:
- redness
- foreign body sensation on the eye surface (gravel, sand feeling, grittiness)
- burning, stinging, scratchiness sensation
- photophobia (light sensitivity)
- mucous discharge on the lids
- eye irritation from smoke or wind
- difficulty wearing contact lens
- excess tearing
What exactly is the tear film?
A film of tears is spread over the surface of the cornea each time the eyelids open and close (Figure 1). Tears are much different then water and are made of an oil layer, a water layer, and a mucous layer (Figure 2). Each component is important for a stable tear film. If one of the components is deficient, the tear film will be unstable resulting in ocular irritation. The oil layer is produced by the meibomian glands of the eyelid and not only smoothes the tear surface but reduces evaporation of tears. The middle layer is a watery layer produced by the main lacrimal gland and accessory lacrimal glands (glands of Wolfring and Krause) located in the conjunctival fornices. This layer cleanses the eye surface and rinses away foreign particles. The inner most tear layer consists of mucous produced by the goblet cells of the conjunctiva. Mucous allows the watery layer to spread evenly over the surface of the eye and help the tears to remain wet. Without mucous, tears would not adhere to the eye.
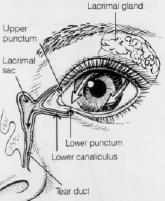
Figure 1 Tears are made in Lacrimal gland and drained out via the nasolacrimal system (tear duct).
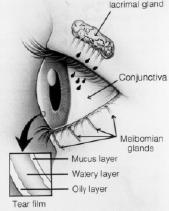
Figure 2 Components of the tear layer.
What are some of the causes of a dry eye?
Tear production normally decreases as we age. Although a dry eye can occur in both men and women at any age, women are most often affected (especially after menopause).
A dry eye can also be associated with arthritis and accompanied by a dry mouth. People with dry eyes, dry mouth and arthritis are said to have a condition called Sjogrens Syndrome. This entity is characterized by infiltration of the lacrimal glands and salivary glands with lymphocytes causing secondary compromise of the gland function. Women are more commonly involved then men. Patients with primary Sjogrens have non-classifiable systemic disease and symptoms that may include anthralgia, myalgia, or fatigue. Patients with secondary Sjogrens have a distinct autoimmune disease such as Rheumatoid Arthritis, Scleroderma, or Systemic Lupus Erythematosus. Diagnosis and treatment of underlying systemic immune disorders may decrease morbidity and may even be life saving.
Rosacea is a disease of the skin and eyelid that is seen more frequently in fair skinned individuals, but can be found in all races. Characteristic facial skin changes include erythema, telangiectasia, pustules, prominent sebaceous glands, and rhinophyma. Meibomian gland dysfunction develops in the majority of patients with rosacea.
Stevens Johnson Syndrome, Ocular Cicatricial Pemphigoid, chemical injuries, Herpes Simplex conjunctivitis, and other cicatrizing processes involving the conjunctiva may lead to scarring of the conjunctiva and resultant dry eyes secondary to an unstable tear film (goblet cells affected).
Blepharitis (inflammation of the meibomian glands) is extremely common and associated with small bits of debris along the lash roots. With inflammation of the meibomian glands, the oil component of the tear film is affected. With a disruption of the oil component of the tears, an unstable tear film may result. Blepharitis may cause symptoms of irritation on its own but also is commonly associated with another disruption of the tear film (i.e. decreased production of the water component from the lacrimal gland). Patients that have both blepharitis and decreased lacrimal gland production are always worse than those with just one or the other.
A variety of common medications (prescription and over the counter) can cause a reduction in tear formation and as a result, dry eyes. Examples include diuretics, beta-blockers, antihistamines, anticholinergics, psychotropics, some sleeping pills, and some pain killers. Since these medications are generally required, some level of dry eye may have to be tolerated by the patient.
Why do some patients with dry eye have excess tearing?
Excess tearing from “dry eyes” sounds illogical, but if the tears responsible for maintenance lubrication (basic tear secretion) of the cornea do not keep the eye wet enough, the eye becomes irritated (even though the patient may not feel this). When the eye senses dryness, a message is relayed to the brain (a reflex pathway) and then to the lacrimal gland to produce extra tears. This extra load of tears come on to the eye surface and overwhelms the tear drainage system. As a result, they end up on the cheeks. This situation is referred to as “reflex tearing” and is quite common. Treatment of reflex tearing involves lubricating the ocular surface (with artificial tears) so this reflex pathway is not triggered. This same mechanism (reflex tearing) explains why people tear when they get something in the eye (e.g. eyelash). The excess tear production often flushes out the foreign body (lash).
Diagnostic Tests
Tear break up time
The tear breakup time is determined by instilling fluorescein into the inferior conjunctival cul-de-sac and then assessing the stability of the precorneal tear film. The time lapse between the last blink and the appearance of the first randomly distributed dry spot on the cornea is the tear break up time. Dry spots that appear in less than 10 seconds are considered abnormal. Tear break up time is rapid for both aqueous tear deficiency and meibomian gland disease.
Schirmer Test
The Schirmer test is performed by placing a narrow piece of filter paper into the inferior conjunctival cul-de-sac. Schirmer testing may be performed with or without the use of topical anesthesia. Applying topical anesthesia eliminates reflex tearing in most individuals and is the preferred method. After applying 1 or 2 drops of topical anesthetic, the conjunctival cul-de-sac is gently blotted to remove excess fluid. The Schirmer filter paper is then inserted into the conjunctival cul-de-sac and rests on the lid margin. Generally less than 5 to 10 mm of wetting after 5 minutes is suggestive of a dry eye.
Ocular surface dye staining (Rose bengal, fluorescein)
Rose bengal is a topical dye that will stain devitalized epithelial cells. After applying Rose bengal, the ocular surface (cornea and conjunctiva) is examined for stained areas. Fluorescein dye stains degenerating or dying cells where there is sufficient disruption of intercellular junctions to allow penetration of the dye to the cornea stroma. An exposure-zone of fluorescein stain is often observed in the lower one third of the cornea.
Treatment of dry eyes
While most forms of dry eye cannot be prevented, appropriate treatment usually reduces symptoms while reducing or preventing permanent corneal problems.
1. Eliminating exogenous factors
For those cases induced by medication (antihistamines, diuretics) and environmental factors (e.g. sitting near an air conditioner or heater), elimination of the offending drug or modification of the patient’s home or work environment may be curative.
Tears evaporate like any other liquid. In the winter, a warm dry environment of ten aggravates the dry eye. Humidifying the air with a cold mist or steam humidifier often eases some of the ocular irritation experienced by a dry eye patient.
2. Tear Supplements
There are a variety of artificial tears available to supplement the patient’s tear film. They all lubricate the eyes and help maintain the tear film. Some patients prefer one brand over another. Generally they should be used at least 4 times daily. Using them more often is occasionally necessary for severe cases.
Preservative free artificial tears are available for those individuals sensitive to the preservatives with in the tear sample. Preservative sensitivity is suspected when administration of the standard artificial tear sample causes further ocular irritation, and/or itchiness and burning.
If artificial tears ever y 2 hours are not sufficient to keep the eye comfortable, a thicker (more viscous) artificial tear or a tear gel is used. Tear gels are applied onto the ocular surface in the form of a gel. Over the next minute the gel melts to a thick tear. The tear gel lingers on the corneal surface much longer than a standard artificial tear (40 mins vs. 1-5 mins)
The addition of a lubricating ointment at night is another helpful measure for the dry eye patient. These lubricants (ex. Lacrilube or Hypotears ointment) produce a thick protective layer over the cornea during the night. The ointment is not used during waking hours because it will cause blurry vision.
3. Conserving the tears
Conserving ones own natural tears is another approach and often used when artificial tears or gels are not helping.
Tears flow into the nasolacrimal system via a punctal opening on the medial aspect of the upper and lower lid (Figure 1). These punctal openings may be temporarily blocked by placing dissolvable plugs within the canaliculus or blocking the opening of the puncta with a non-dissolvable tear plug. The openings can also be permanently closed with the application of cautery to the punctal opening or laser to the opening.
4. Other helpful measures
Avoid sitting near fans, air conditioners, and forced air heating ducts. Adjusting computer screens to avoid reflections or lowering the computer screen to decrease the lid opening by having the patient look down at the screen also may be helpful. Scheduling regular breaks while reading may decrease the dryness associated with such activities.
Wrap around glasses may reduce the drying effect of the wind. A smoke filled environment can be particularly bothersome to the dry eye patient and should be avoided.
Patients with systemic disease such as Sjogrens Syndrome or Rheumatoid Arthritis should be managed in conjunction with a medical specialist, as control of the systemic disease often influences the dry eye.
In summary – DRY EYES ARE COMMON. Although this problem more commonly affects the aging female it can occur at any age, male or female (it may even be congenital). Dry eye symptoms can wax and wane depending upon the etiology of the disease process as well as the environment (winter vs. summer). The dry eye condition is a life long process and may be progressive leading to increasing eye discomfort and requiring multiple visits to the physician. While the symptoms often improve with treatment, the disease usually is not curable and the chronicity of the disease may lead to patient frustration. One needs to learn how to live with the condition as it rarely resolves on its own.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.

LOOK YOUNGER, FEEL REFRESHED
Contact us today to discover how we can help you achieve a more youthful, refreshed look.



