Volume 6 • Issue 2
Assessment of the Patient with Droopy Lids

by David R. Jordan
M.D., F.A.C.S., F.R.C.S.(C)
INTRODUCTION
Droopy eyelids are common in the aging population and may involve one or both lids. What one physician refers to as a “droopy eyelid” how-ever, is not always what another is referring to. The drooping appearance may be due to: true “eyelid ptosis”(levator aponeurosis thinning or disinsertion), “excess eye-lid skin” (dermatochalasis), “brow ptosis”, “contralateral eyelid retraction”, “enophthalmos” (sunken eye) or, a combination of the above. The treatments for these various problems are different and it is essential to sort out which of the contributing factors are present in each individual so that an appropriate management plan can be organized.
Eyelid Ptosis
Ptosis (pronounced “toe-sis”) of the eyelids refers to a drooping of the upper eyelid as a result of a problem with the eyelid elevating muscle (the levator). The lid droop may be minimal or it may droop to partially or completely cover the pupil and restrict the superior visual field [Figure 1].
Ptosis may be congenital or acquired. Congenital ptosis is present at birth and is commonly due to a dystrophic levator muscle while acquired ptosis develops with age. The commonest type of acquired ptosis is due to a thinning and/or disinsertion of the levator aponeurosis (that portion of the levator muscle which inserts onto tarsal plate). Other types of acquired ptosis are mechanical (due to a stye, chalazion or eyelid tumor), traumatic (blunt or surgical i.e. post cataract surgery), myogenic (i.e. myasthenia gravis), or neurogenic (i.e. Horners syndrome).
The treatment for eyelid ptosis (with the exception of myasthenia) involves an advancement of the levator aponeurosis onto the tarsal plate, with a resultant lifting of the eyelid.

Figure 1– True eyelid ptosis as a result of levator thinning. The eyelids are covering part of the pupil.
Excess Eyelid Skin (Dermatochalasis)
Excess eyelid skin that hangs over the eyelid margin also gives the eyelid a droopy appearance, but for a different reason than true eyelid ptosis. With dermatochalasis, it is the skin hanging over the lid margin that is responsible for the drooping appearance [Figure 2a]. The underlying eyelid height may be normal or low depending upon whether any true eyelid ptosis exists. The way to assess this situation is to gently raise the excess lid skin off the eyelid [Figure 2b] and measure the lid height either with a ruler or by shinning a light at the eye from a distance of 2 feet or so. A normal eyelid fissure height is generally about 10 mm. By shinning a pen light toward the patient from a two foot distance a light reflex is created on the cornea. The distance between the light reflex and the upper lid margin is termed the “margin to reflex distance” or MRD. The MRD is usually 4 mm. A value of 1 or 2 is abnormal and indicates a true ptosis of the eyelid is also present.

Figure 2– Excess eyelid skin responsible for drooping appearance of lids.

Figure 3– When the excess eyelid skin on the patient’s right upper lid is gently lifted, the true eyelid height is found to be at a normal level.
Treatment of dermatochalasis involves removal of excess skin and fat on the eyelid (blepharoplasty). The levator aponeurosis is not touched unless of course the patient has a true lid ptosis as well. In this latter situation the appropriate surgery would then involve a levator aponeurotic advancement in conjunction with removal of excess skin and fat (blepharoplasty).
Brow Ptosis
A man’s brow is generally more full, straighter and rests at level of the orbital rim, while a lady’s brow is thinner, curved and generally sits above the orbital rim.
As we age the fibrous connective tissue structures within our facial tissue becomes lax and as a result tissues begin to sag due to gravitational forces pulling downward. A gradual migration of the eyebrow inferiorly is a result of these aging changes. As the eyebrow moves downward the excess eyelid skin appears to be more than it actually is and gives rise to a droopy eyelid [Figure 3a]. This phenomenon can be assessed by finding where the brow is in relation to the orbital rim. If the aging male or female brow is sitting below the rim, gently elevating it to the rim level or slightly above will elevate some of the excess eyelid skin (that component contributed by the droopy brow) so that one can get an appreciation of the true excess eyelid skin and true eyelid height [Figure 3b].

Figure 3a– Severe brow ptosis giving a droopy appearance to lids. The brows are below the orbital rims.
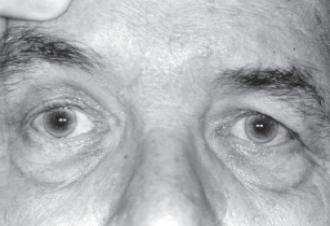
Figure 3b– When the patients right brow is elevated to a normal level, the true eyelid height is found to be normal and there is only a small degree of excess lid skin (dermatochalasis).
It is extremely important to sort out whether the brows are playing a role in the “droopy eyelid”. If the patient with brow ptosis and excess lid skin simply has the eyelid skin removed, the droopy eyelid may not be corrected as the brows will still be low and may appear to be sitting in the upper lid. In fact, the brow droop may even appear more noticeable following the eyelid skin removal since removal of the lid skin may pull the brow further downward (into the lid). Sometimes brow elevation on its own, by lifting the excess lid skin upwards, is all that is needed to correct the so called droopy eyelid. More commonly the patient with brow ptosis has a combination of brow ptosis and excess lid skin. In this case brow elevation on its own will only partially correct the excess lid skin, and a brow elevation with upper lid skin/fat removal (blepharoplasty) is more appropriate. It is also possible for the patient to have brow ptosis, dermatochalasis and true lid ptosis all at once. In this situation the patient requires brow elevation, blepharoplasty, and levator advancement surgery. Simply doing one will not correct the others.
Brow elevation surgery can either be done immediately above the brow hairline, in the mid-forehead, along the temporal hairline or endoscopically behind the frontal hairline, depending upon the patient’s facial features.
Contralateral Eyelid Retraction
Sometimes a patient presents with a drooping upper lid that actually has a retracted opposite upper eyelid. This situation is most commonly due to unrecognized Thyroid eye disease (Grave’s disease). The so-called droopy eyelid is only droopy in comparison to the opposite lid which is actually retracted superiorly. The lid retraction may be partially hidden by excess skin [Figure 4a] (dermatochalasis) and only becomes apparent if the lid skin is gently lifted [Figure 4b]. This type of patient requires a thyroid work-up including a medical history looking for systemic signs, family history of others with thyroid disease and a TSH test. If all are negative they need to be followed for several months as lid retraction is occasionally the initial sign of thyroid eye disease, despite a normal TSH test. Systemic hyperthyroidism may not show up for months or years later.

Figure 4a– Patient presented with ptosis of her right upper lid. It is actually the left upper lid that is too high (partially hidden by excess skin).

Figure 4b– The left upper lid retraction becomes more obvious as one gently lifts the skin on the left upper lid upward by manually elevating the left brow.
Enophthalmos and Droopy Eyelids
Enophthalmos refers to a sunkeness of the orbital tissue. It is not uncommonly seen following a blow to the orbit causing an orbital fracture. The fractured bones allow an increase in the orbital volume and as a result the eye moves posteriorly. As the eye moves posteriorly the upper lid may fall creating a droopy lid appearance.
The droopy lid appearance is a direct result of the expanded orbital volume. This situation is often referred to as a pseudo-ptosis (a false ptosis since the lid isn’t the problem).
To correct the false eyelid ptosis one needs to correct the enophthalmos. Correction of the enophthalmos requires restoration of the orbital volume. During floor fracture repair the orbital tissue that is herniated into the maxillary sinus, is repositioned into the orbit. A plate of some variety (supra-mid, Teflon, porous polyethylene, titanium mesh) is used to cover the bony defect, prevent re-herniation of the tissue and allow a restoration of the orbital volume.
Enophthalmos may have a more sinister problem associated with it. It is not uncommon for metastatic breast cancer to show up in the orbit 20 years later (even following appropriate treatment of the breast cancer), with a pseudo-ptosis as the result of enophthalmos. The matastatic breast cancer cells create a fibrosing reaction within the orbital tissue. As a result the eye is pulled posteriorly (enophthalmos) and the eyelid falls giving the appearance of an eyelid ptosis [Figure 5].

Figure 5– Patient has a ptosis involving her right upper lid as a result of a metastatic tumor in the right orbit pulling the eye back (enophthalmos).
Summary Examination of the patient with a “droopy eyelid” should involve an assessment of the:
1. eyelid height (true ptosis and contralateral eyelid retraction)
2. brow position
3. eyelid skin (dermatochalasis)
4. enophthalmos
Appropriate treatment can only be performed if the surgeon knows the contributing factors and corrects them.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.