Volume 9 • Issue 1
Canalicular Lacerations

by David R. Jordan
M.D., F.A.C.S., F.R.C.S.(C)
INTRODUCTION
Trauma to the eyelid may occur with blunt or penetrating injuries due to flying objects, motor vehicle accidents, tree branches, dog and cat scratches/bites, etc. Lacerations involving the canalicular system may occur with any of these injuries, but unfortunately are often overlooked on initial examination (Figure 1a, 1b).
The first step in treatment of an eyelid laceration is a careful history. It is important to appreciate the mechanism of injury as well as the force and velocity at which the object approached the eye area. In all periocular/eyelid trauma cases, it is essential to document the visual acuity and ocular status (cornea, anterior chamber, iris, red reflex, fundus, etc.) in order to rule out damage to the globe prior to treatment of the lid abnormality. Once this has been done, the lid laceration and canalicular system can be examined.

Figure 1a – Medial eyelid laceration – sutured together in emergency room.
Anatomy of the Canalicular System
The lacrimal papillae are very small, pale elevated mounds located along the mucocutaneous junction of the medial eyelid near the medial canthus/caruncle area. In the center of each papilla is a punctum that opens into the canalicular system. The punctal openings should not be seen unless the eyelids are slightly everted. If they are easily seen, a degree of punctal ectropion exists and may sometimes explain a patient’s tearing complaint. The punctal openings are approximately 0.3 mm in diameter and the superior puncta should be in the same vertical line as the inferior puncta. When the lids close they should approximate each other. The puncta are the entrance way into the canalicular system.
The canaliculi are each about 10 mm long and have a 2 mm vertical portion followed by an 8 mm horizontal portion. In most individuals the two horizontal components meet just prior to joining the nasolacrimal sac. In medial eyelid the canaliculi are immediately subcutaneous, and as they approach the nasolacrimal sac are somewhat protected by the anterior limb of the medial canthal tendon, which lies anterior to them.
Canalicular Lacerations – Tips to Diagnosis
Lacerations involving the canaliculi are the most common type of trauma to the lacrimal system. The canaliculus may be injured by a direct penetrating injury (i.e. tree branch) to the medial lid or, by an indirect injury to another part of the lid, for example, a blunt blow to the lateral lower eyelid (i.e. fist) may actually tear the medial eyelid at the canalicular level. Thus, canalicular lacerations may occur by direct (penetrating) or indirect (nonpenetrating-stretching) blows.
In a person presenting with an obvious eyelid laceration ask yourself: Where is the laceration in relation to the pupil? For any eyelid laceration medial to the pupil, the canaliculus may be involved and the examining physician must specifically look to see whether it is or not.
Sometimes canalicular injuries are subtle, and although the history is there, along with signs of trauma over the canaliculus, one cannot be sure. In these instances – a gentle punctal dilation and probing of the canalicular system with a Bowman lacrimal probe may be the only way to confirm the canalicular laceration (Figure 2a, 2b).

Figure 2a – Cat scratch to right lower lid. Laceration is medial to the pupil.

Figure 2b – Right lower lid canaliculus is involved and required repair.
Do all isolated canalicular lacerations (i.e. monocanalicular
lacerations) need repair?
The need for surgical repair of a single severed lacrimal canaliculus is somewhat controversial, largely because the relative roles of the upper and lower canaliculi have not been clearly established or appreciated. Some articles on this subject1,2,3,4 have suggested the superior canaliculus is sufficient (by itself) to keep patients symptom free, whereas, other papers have suggested the lower canaliculus is more important to tear drainage5,6,7,8,9,10 to the point that Werb10 concluded “conservation of the inferior canaliculus is for tear drainage and the superior canaliculus for the ophthalmologist”.
To appreciate the relative roles of the upper and lower canaliculi in tear drainage it is essential to review reports on this subject matter (which are few in number).2,3,11,12 Reviewing this literature, it is fair to state that traumatic loss of a single canaliculus does not necessarily lead to symptoms of tearing.5,13,14,15 It is also fair to state that tear drainage studies show that both superior and inferior canaliculi play a role in tear drainage.2,3,11,12 Based on these studies it appears that some individuals may be primary tear drainers through their upper system and only minimally through their lower system while others may be primary tear drainers through their lowers and only minimally through their upper. Some individuals may drain their tears quite satisfactorily through either the upper or lower canaliculus when the other is blocked, while others may not.2,3 When faced with a monocanalicular laceration (upper or lower), one does not know whether the patient will remain symptom free with one functioning canaliculus, they may not. Some patients may feel reassured that constant tearing will rarely result from a single obstructed canaliculus (especially if there are medical problems to make surgery hazardous).2 On the other hand, there may be symptoms (although mild and intermittent such as a watering eye or mildly blurred vision when walking outside or driving a car with the window open) in 50%.2,3 We agree with Linberg that few of these patients (monocanalicular lacerations) are willing to accept a 50% risk of even mild, intermittent symptoms.
It is for this reason, in conjunction with the known excellent success rate associated with modern microsurgical techniques for canalicular repair (>95%)16,17,18 that I suggest the following: both upper and lower canaliculi are important in tear drainage and when faced with a monocanalicular laceration (upper or lower), an attempt should be made to repair it, following the fundamental repair principles of 1) re-approximation of the severed ends, 2) endocanalicular support with silicone tubing, and 3) utilization of a technique that is atraumatic to the uninvolved part of the nasolacrimal system.18 There are several canalicular repair techniques available depending upon the surgeon’s preference. These include monocanalicular intubation, bicanalicular intubation of the canalicular system using a round tipped eyed pigtail probe (Figure 3) and, bicanalicular nasolacrimal duct intubation using silicone stents through the canalicular and nasolacrimal duct.
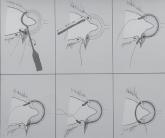
Figure 3
Technique for Canalicular repair using the round tipped eye pigtail probe.
For those ophthalmologists, plastic surgeons, etc. that don’t feel comfortable repairing lacerated canaliculi, the patients can easily be transferred to another centre where it may be repaired, anytime within the first 7-10 days after injury. Similarly, in the patient medically unfit for surgery at the time of their injury, the canalicular laceration can be left for 7-10 days if necessary. This author has personally repaired numerous missed canalicular lacerations within this time frame (7-10 days) with excellent results (>95%anatomical and physiological success). The soft tissue sutures are removed in the area of the canalicular laceration and the wound is gently teased apart. The canalicular laceration is then repaired following the previously stated fundamental principles.
Certainly, there will be those occasional patients that one is unable to repair the severed canaliculus. In these cases it is nice to know that there is still a good chance the patient will be free of tearing symptoms most of the time with only one remaining canaliculus. However, I feel this is more appropriate management than suggesting “non repair of monocanalicular lacerations is a valid approach that results in little or no morbidity”.
In summary
1. Canalicular lacerations may occur by direct penetrating injuries (i.e. tree branch), or indirect blunt injuries to the lateral lid that tear the canaliculus medially
2. For any eyelid laceration medial to the pupil the examining physician should ask “Is the canaliculus involved?” (Figure 4)

Figure 4
Laceration central to the pupil and involving canalicular.
3. An attempt should be made to repair all canalicular lacerations (superior or inferior) and if one does not feel comfortable doing so – transfer the patient within 7-10 days to someone experienced with canalicular lacerations
4. Principles of repair include: 1) re-approximation of severed ends, 2) endo-canalicular support with silicone tubing, and 3) utilization of a technique that is atraumatic to the uninvolved part of the nasolacrimal system.
References
1. Smit TJ, Mourits M. Monocanalicular lesions: to reconstruct or not. Ophthalmology 106:1310-1312;1999.
2. Linberg JV, Moore CA. Symptoms of monocanalicular obstruction. Ophthalmol 95:1077-1079, 1988.
3. Canavan Ym, Archer DB. Long-term review of injuries to the lacrimal drainage apparatus. Trans Ophthalmol Soc UK 99:201-4, 1979.
4. Ogut MS, Baubek T, Kazokoglu H. Assessment of tear drainage by fluorescein dye disappearance test after experimental canalicular obstruction. Acta Ophthalmol (Copenh) 71:69-72, 1973.
5. Welham RAM. The immeduate management of injuries to the lacrimal drainage apparatus. Trans Ophthalmol Soc UK 102:216-7, 1982.
6. Weber R, Draf W. Reconstruction of lacrimal drainage after trauma or tumor surgery. Am J Otolaryngol 15:329-35, 1994.
7. Bodian M. Repair of occluded lower canaliculus. Arch Ophthalmol 95:1839-40, 1977.
8. MacGillivary RF, Stevens MR. Primary surgical repair of traumatic lacerations of the lacrimal canaliculi. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 81:157-63, 1996.
9. Saunders DH, Shannon GM, Flanagan JC. The effectiveness of the pigtail probe method of repairing canalicular lacerations. Ophthalmic Surg 9(3):33-40, 1978.
10. Werb A. Panel discussion on the lacrimal system. In Smith B, Converse JM, Wood-Smith D, Obear MF, eds. Plastic and Reconstructive Surgery of the Eye and Adnexa: Proceedings of the Second International Symposium St Lousi. CV Mosby 182, 1967.
11. Jones LT, Marquis MM, Vincent NJ. Lacrimal functions. Am J Ophthalmol 73:658-9, 1972.
12. Lemp MA, Weiler HH. How do tears exit? Invest Ophthalmol Vis Sci 24:616-22, 1983.
13. Adams AD. Repair of the torn canaliculae. Trans Ophthalmol Soc UK 98:498, 1978.
14. Meyer DR, Antonello A, Linberg JV. Assessment of tear drainage after canalicular obstruction using fluorescein dye disappearance. Ophthalmology 97:1370-4, 1990.
15. Reifler DM, Management of canalicular lacerations. Survey Ophthalmol 36:113-32, 1991.
16. Dortzbach RK, Angrist RA. Silicone intubation for lacerated lacrimal canaliculi. Ophthalmic Surg 16:639-42, 1985.
17. Hawes MJ, Segrest DR. Effectiveness of bicanalicular silicone intubation in the repair of canalicular lacerations. Ophthalmic Plast Reconstr Surg 1:185-90, 1985.
18. Jordan DR, Nerad JA, Tse DT. The pigtail probe revisited. Ophthalmology 97:512-9, 1990.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.