Volume 8 • Issue 2
Ectropion

by David R. Jordan
M.D., F.A.C.S., F.R.C.S.(C)
INTRODUCTION
Ectropion refers to an outward turning of the eyelid and may be unilateral or bilateral [Figure 1]. It primarily involves the lower lid and only very rarely the upper lid. As the eyelid turns out, the eye often begins to tear since the punctal openings move out of position and are unable to collect tears properly. With further outward turning the conjunctiva becomes red, dry and irritated. If untreated it may cause persistent eye irritation, recurrent tearing and discharge.

Figure 1
Involutional ectropion of the lower lid.
Etiology
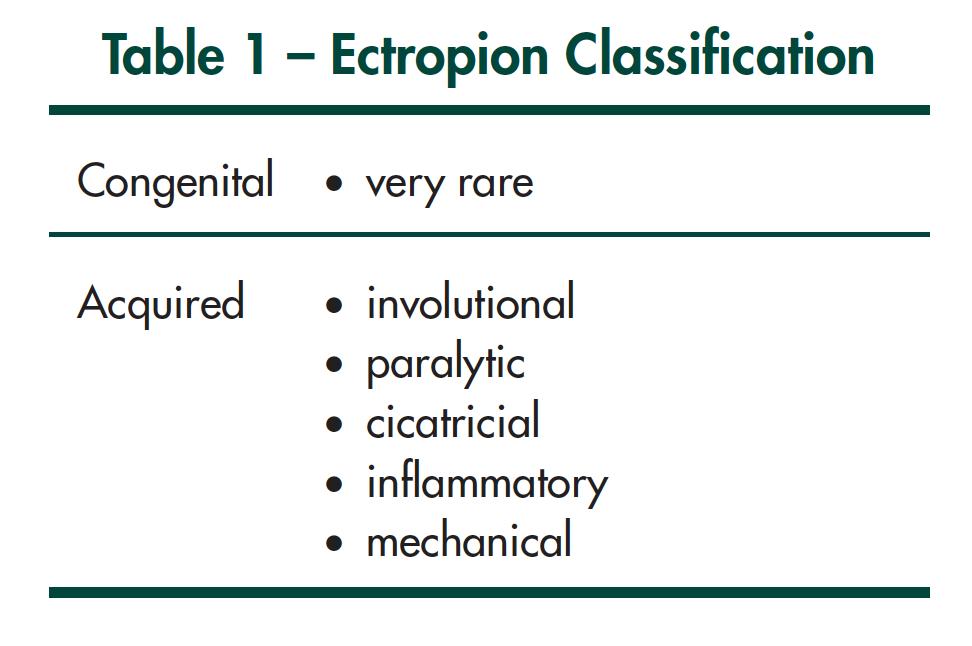
Ectropion may be classified as congenital or acquired. Congenital ectropion is uncommon. Acquired ectropion may be divided into involutional, paralytic, cicatricial, inflammatory or mechanical types [Table 1].
Pathophysiology: Why does the eyelid turn out?
Congenital Ectropion
Congenital ectropion is very rare. When present, it is due to a vertical shortage of skin. This may be seen in congenital skin diseases such as icthyosis. In this condition the lower lid skin keratinization process is faulty which subsequently leads to tight scaly skin that gradually pulls the lower lid over. Blepharophimosis syndrome is a congenital disorder with ptosis, phimosis, telecanthus and lateral lower lid ectropion (secondary to tight lower lid skin). Both conditions are very rare.
Acquired Ectropion
Congenital ectropion is very rare. When present, it is due to a vertical shortage of skin. This may be seen in Involutional Ectropion – is by far the commonest form of ectropion. [Figure 1] The etiology is similar to involutional entropion with laxity of the medial and lateral canthal tendons and thinning of the lower lid retractors (help stabilize the lower lid in the vertical position). The orbicularis muscle however does not ride upward as it does in entropion. In ectropion the orbicularis has a normal or decreased tone. In addition, ectropic lids have tarsal plate heights that are greater in vertical height than normal lids. Thus, in the aging lax lid there is loosening or thinning of the medial and lateral canthal tendon tissue as well as the lower lid retractors. Whether the eyelid turns in or out often depends upon the tone of the orbicularis muscle as well as the height of the tarsus. A weak orbicularis (e.g. seen as a result of aging or in 7th nerve palsy) will allow the aging lid to fall over. A higher tarsal plate in the face of a weak orbicularis will also have a tendency to fall outward whereas shorter tarsal plates will have a tendency to turn inward (providing the orbicularis tone is active – as is the case with entropion).
Paralytic ectropion – follows temporary or permanent seventh nerve palsy. When the orbicularis muscle loses its tone the lid loses an important support structure and as a result the lid falls outward. Poor blinking ability and incomplete lid closure, lead to corneal exposure, tearing, chronic eye irritation and corneal ulceration.
Cicatricial ectropion – involves a scarring process of the skin with resultant shortening of the skin. It may be seen secondary to thermal/chemical burns or trauma [Figure 2].

Figure 2
Cicatricial ectropion secondary to a scar, pulling the lid over.
Inflammatory ectropion – is associated with inflammation of the skin as seen in acute allergic reactions to topical drops or ointment, atopic dermatitis, eczema or occasionally rosacea [Figure 3]. Each of these conditions may cause tightening of the lid skin which may then pull the lid outward. If the process becomes chronic the eyelid will remain permanently turned out due to tight lower lid skin. In the early phase however it may be reversible with anti-inflammatory steroid creams.
Mechanical ectropion – bulky tumors of the eyelid may pull the lid over. Similarly, poorly fitting eye glasses sitting on a lax lid may pull the eyelid outward.

Figure 3
Inflammatory ectropion – secondary to severe atopic dermatitis of the lower lid.
How is Ectropion treated?
Ectropion treatment for the most part is surgical. The only types that may be amenable to temporizing measures are the inflammatory variety and the paralytic form (secondary to 7th nerve palsy). If there is active inflammation of the skin (ex atopic dermatitis, allergy) a steroid cream may settle the inflammation and allow the ectropic lid to return to a normal position. In the 7th nerve palsy patients, the use of lubricating drops and ointment combined with taping the involved lids closed at night may be successful in keeping the eye comfortable for a short time period while working on recovery of function. If the 7th nerve function recovers the lid should return to normal.
Most ectropions, however, will require surgery. Surgery is generally done as an outpatient under local anesthesia. The surgery involves tightening the lower lid and turning the lid margin back to its normal position. If one eyelid is operated on, patients are usually patched overnight. If both eyelids are involved, cool compresses over each eye rather than eye patches are used. Antibiotic drops and ointment are required for about 7-10 days post surgery. Pain is not a major factor. Most people will have some mild discomfort in the first one to two days. Patients can return to their usual daily activities within 2-3 days.
Complications
Ectropion surgery is successful in over 95% of patients. Recurrence occasionally occurs over 2-10 years but is uncommon. If the ectropion does recur, surgery can always be done again. Occasionally an infection occurs at the site where sutures are placed, oral antibiotics and warm compresses are required if this occurs.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.