Volume 8 • Issue 1
Entropion

by David R. Jordan
M.D., F.A.C.S., F.R.C.S.(C)
INTRODUCTION
Entropion refers to an inward turning of the eyelid [Figure 1]. It may be unilateral or bilateral and only rarely involves the upper lid. Entropion commonly occurs in the aging population but may occasionally be seen in the child or middle aged adult. When the lid turns in, the eyelashes and/or lid skin rub against the cornea, creating an irritated red eye with associated photo-sensitivity. If untreated it may lead to corneal ulceration and infection.

Figure 1
Involutional Entropion of the lower left lid.
Etiology
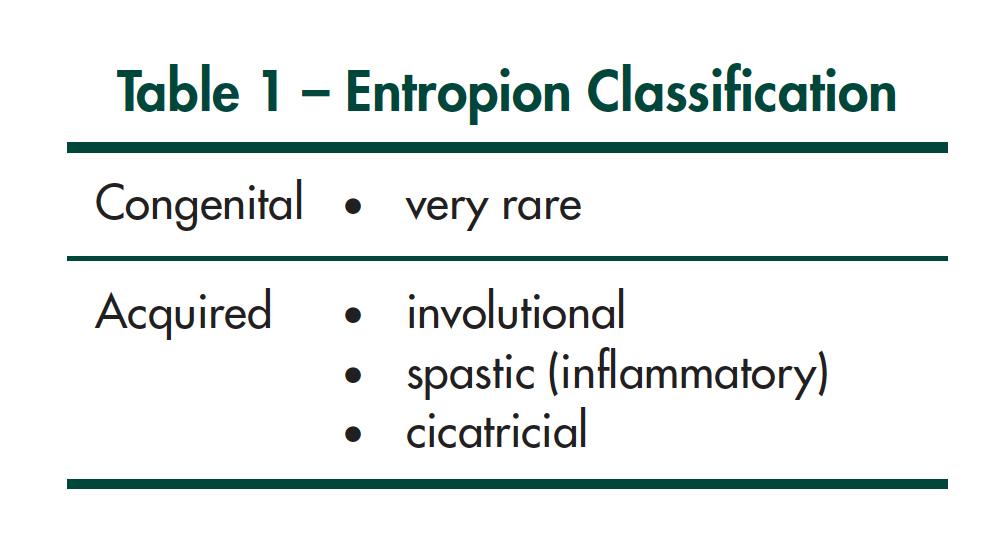
Entropion may be classified as congenital or acquired.
Acquired entropion may be divided into involutional, spastic (or inflammatory), and cicatricial [Table 1].
Pathophysiology – Why does the eyelid turn in?
Congenital Entropion
Congenital entropion is very rare. The etiology is felt to be secondary to a faulty development of the lower eyelid retractor system. The lower lid retractors are responsible for stabilizing the lower lid in the vertical position. With weak or absent lower lid retractors the orbicularis may roll the lid inward causing entropion. A more frequently occurring entity that rolls the lashes inward (seen commonly in Asian children) is epiblepharon. In epiblepharon a fold of skin and lower lid muscle roll upward pushing the lashes toward the cornea especially on down gaze [Figure 2]. If the lashes touch the cornea, the child experiences ocular discomfort and photosensitivity. The difference between congenital entropion and epiblepharon is that in entropion the tarsal plate is inverted whereas in epiblepharon the tarsal plate remains in an upright position. They both however lead to lashes rubbing on the cornea.

Figure 2
Epiblepharon – a fold of skin and muscle is seen pushing the lashes toward the cornea.
Acquired Entropion
Involutional entropion – is the commonest form of entropion in the adult and commonly seen in the aging population [Figure 1]. The pathophysiology is related to a loss of supportive structures within the lower lid. With age, the medial and lateral canthal tendons become lax. The lower lid retractors also become thin and attenuated. Entropic lids have also recently been found to have a shorter tarsal plate height than normal, which is another predisposing factor to inward lid rotation. As these aging changes occur, the tarsal plate begins to lose stability. With an active orbicularis tone there may be over-riding of the pretarsal orbicularis superiorly and as a result the lid margin is rolled in, resulting in entropion.
Acute spastic or inflammatory entropion – follows ocular irritation or inflammation. It may occur following a foreign body on the cornea which subsequently leads to ocular discomfort, photosensitivity and excess lid squeezing. It may also be seen with intraocular inflammation such as iritis. In addition it may occur following intraocular surgery (ex. Cataract surgery) in a patient who has unrecognized or mild involutional lid changes. In each of the above situations, the eye irritation causes sustained lower eyelid squeezing (orbicularis muscle contraction) which causes the lid margin to roll inward. Corneal irritation secondary to lashes rubbing on the cornea causes further irritation and inflammation which subsequently causes further eye irritation and orbicularis spasm.
Cicatricial entropion – is a result of scarring on the conjunctival side of the lower lid. A variety of conditions may lead to this including, trauma,cicatricial pemphigoid, Stevens Johnson Syndrome, trachoma, herpes, thermal or chemical burns. As the conjunctival tissue contracts the lid margin is pulled inward [Figure 3].

Figure 3
Cicatricial entropion of right upper lid and right lower lid.
How is Entropion treated?
The treatment, for the most part, involves surgery. A temporizing measure which may correct the lid position in the short term, is taping the lower lid skin to the cheek in order to evert the lid margin. Surgical tape or the sticky part of a bandaid, placed from the lower lid to the upper cheek area, will evert the lid and relieve the corneal irritation from the lashes. In a spastic or inflammatory entropion (ex. post cataract surgery) this may occasionally be all that is needed. However, it is not unusual for the entropion to continue and require corrective surgery.
A variety of techniques exist to correct entropion. With the exception of children, surgery is done under local anesthesia as an outpatient. Dissolvable sutures are preferred and the lid heals over the next few weeks. If one eyelid is operated on, patients are often patched at night. If both eyelids are involved, cool compresses are placed over each eye rather then eye patches. They are used 3 or 4 times daily over the first few days. Antibiotic drops and ointment are required for about 7-10 days post surgery. Pain is not a major factor. Most people will have some mild discomfort in the first one to two days. Patients can generally return to their usual daily activities within 1-3 days.
With cicatricial entropion – surgery is also required and is often more involved than in involutional entropion. In mild cicatricial cases a tarsal rotation procedure may be helpful. In more severe cases a tarsal fracture or lid splitting procedure with mucous membrane grafting may be required.
Complications
Entropion surgery is successful in over 95% of patients. In some patients, a recurrence will occur over 2-10 years and surgery may be required again. Occasionally an infection occurs at the site where sutures are placed requiring antibiotics. All patients are on topical antibiotic drops and ointment post-op to try and avoid this.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.