Volume 10 • Issue 3
Excess Eyelid Blinking

by David R. Jordan
M.D., F.A.C.S., F.R.C.S.(C)
INTRODUCTION
Normal individuals have at least 3 different behavioral patterns of blink rate. The normal blink rate is higher during verbal conversation compared with rest, and slowest during reading. Blinks occur, on average, approximately 15 times per minute in the adult patient. Blinking is virtually absent at birth and increases steadily until adolescence, when it plateaus and is maintained throughout adult life. In an infant, blinking may occur as infrequently as one to two times per minute. Spontaneous blinking occurs even in blind eyes and is not dependent on visual stimulation.
The patient with excess blinking on one or both sides may have one of the following:
Anterior Segment irritation
Any disorder that produces irritation of the ocular surface or photophobia may be associated with an increased blink rate. For example, severe dry eyes, inturned eyelashes (trichiasis), iritis or scleritis, foreign bodies on the cornea or in the cunjunctial fornix (eyelash, sand, metal fragment from a power tool, etc.) may cause increased blinking.
Habit Spasms or facial tics
Habit spasms or facial tics are repetitive mannerisms of variable frequency involving any number of facial muscles. An eye-blinking tic most commonly presents in childhood as a rapid, exaggerated, coordinated contraction of the orbicularis oculi. Boys are more common only involved than girls and the increased blinking is usually bilateral. The blinking can be voluntarily controlled to some degree, but it often increases in frequency when the individual is bored, tired, or anxious. There may occasionally be other facial twitches present as well. There is little functional visual impairment, and the facial tic typically disappears spontaneously after a duration of weeks to years.
Myokymia
Myokymia is a localized muscle twitch in the eyelid. It is characterized by an involuntary, fine, muscle contraction involving a portion of the orbicularis oculi muscle or other facial muscles. It is often described as a flickering of one eyelid occurring intermittently throughout the day. It tends to occur in young ( 20’s – 30’s), healthy individuals and may last minutes, hour or days. There may be a history of excessive physical exertion, fatigue, lack of sleep, stress or excessive caffeine consumption. It may also be seen after almost any type of eyelid surgery.
Myokymia generally requires no treatment as it commonly resolves spontaneously. Obtaining adequate sleep, reducing caffeine intake and decreasing stress are helpful. If the twitches persist on a daily basis for several weeks, a mild muscle relaxant or an injection of botulinum toxin can be used. Botulinum toxin is extremely effective.
Aberrent Regeneration following Bells Palsy
With Bells Palsy, the facial nerve, loses function. During the regenerative or healing phase, the nerve often regenerates in an abnormal way. This aberrant regeneration is manifest in several ways. The upper and lower eyelid on one side may partially close or twitch during conversation and chewing. Alternatively, there may be excess tearing while chewing food.
The most effective treatment for aberrant regeneration involves botulinum toxin injections. Botulinum toxin injected in minute quantities into the abnormal twitching muscle fibers, will significantly weaken the muscle fibers and decrease the eyelid closure and eyelid twitching. By injecting botulinum into the lacrimal gland the excess tearing during chewing can also be improved.
Benigh Essential Blepharospasm
The term “Blepharospasm”, literally means spasm of the eyelids, and has numerous causes. For example, a foreign body on the cornea, severe dry eyes, iritis or scleritis are each associated with ocular irritation and photosensitivity. This may lead to an increased blink rate or in some cases, excess squeezing of the eyelid muscles (“blepharospasm”). “Benign Essential Blepharospasm (BEB)” however, is a rare condition in which there is involuntary blinking of the eyelids as well as episodes of eyelid closure (spasms) that may be forceful and sustained (5-10 seconds). In contrast to the patient with a corneal foreign body where the cause of the excess blinking is known, the cause of Benign Essential Blepharospasm is unknown. The episodes of excess blinking and eyelid spasms are completely uncontrollable (Figure 1a and 1b). Benign Essential Blepharospasm is a type of Dystonia: a term used to describe abnormal, involuntary, sustained muscle contractions and spasms involving various parts of the body (e.g., torticollis, writers cramp, etc.).

Figure 1a – BEB patient – eyes are open.

Figure 1b – BEB patient with episode of eyelid spasms.
Benign Essential Blepharospasm most commonly affects individuals over the age of 50, with females more commonly affected than males. The eyelid blinking and spasms occur bilaterally. BEB usually begins with an increased blink rate and with time, progresses to episode of forceful eyelid closure (spasms) that may last for 5 to 15 seconds, occurring frequently through out the day. The eyelid spasms in BEB are unpredictable and occur at any time throughout the day. At times the patient may appear to have normal eyelid movement whereas, at other times the patient develops excess blinking and spasms with forceful eyelid closure. Many individuals report that bright lights, stress, fatigue, watching television and driving make the spasms worse whereas the intensity of squeezing is relieved by sleep and relaxation. Some patients discover maneuvers such as touching the eyelids, chewing, talking, humming, coughing or rubbing the forehead may allow temporary suppression of the involuntary squeezing.
Some BEB patients will develop other facial spasms such as lip pursing, chin thrusting and various tongue movements. Blepharospasm with areas of lower facial spasm is referred to as the “Miege Syndrome”.
To compound matters further, about 7% of patients with BEB also develop “Apraxia of eyelid opening”. Apraxia of eyelid opening refers to an inability to initiate the act of opening the eyelids, and usually follows an episode of eyelid spasm. It is not associated with contraction of the closing muscles of the eyelids, but rather an inability to activate the opening muscles. The eyelids simply remain closed after an episode of eyelid spasm and the patient is unable to open them for several seconds.
Treatment of Benign Essential Blepharospasm involves:
1) educating the patient about the disease
2) putting the patient in touch with a support group
3) oral medication ( of limited benefit in 5 – 10%)
4) botulinum toxin (extremely helpful)
5) myectomy surgery (primarily used for botox failures or inadequate response to botulinum toxin)
Hemifacial Spasm
Hemifacial Spasm (HFS), like the name implies, is characterized by an uncontrollable twitching of the muscles on one half of the face (Figure 2a and 2b) in contrast to Essential Blepharospasm which involves eyelid spasms bilaterally. Hemifacial spasm is most common in middle age (50’s, 60’s) but can begin at any age. Like Benign Essential Blepharospasm, it is more common in females. HFS usually starts as a mild twitching of the eyelid muscles, most commonly of the lower eyelid. It gradually spreads to involve the upper eyelid and then in time spreads over the face and neck on the same side. The twitches start spontaneously or may be precipitated by talking, tension, or fatigue. It is at first intermittent, but becomes more frequent and more severe as time passes. With time, the patient may develop prolonged contractions of the muscles, closing the eyelids and pulling the corner of the mouth toward the ear. Once prolonged contractions occur, there is often some facial weakness noted as well.

Figure 2a – Normal eyes.
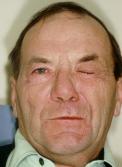
Figure 2b Notice the left side of the face in spasm.
In Hemifacial Spasm, there is an irritation of the 7th nerve in the brainstem. The commonest cause is a blood vessel pulsating against the facial nerve. Rarely, it is due to a tumor pressing on the nerve. All Hemifacial Spasm patients therefore require neuro-imaging such as a CT scan or MRI scan.
Treatment of HFS in the early phase is occasionally improved with oral medication such as a muscle relaxant. The most effective, but temporary improvement comes with botulinum toxin injections. The most definitive treatment involves neurosurgery to place a Teflon sponge between the artery and seventh nerve. This micro-vascular decompression is referred to as the “Janetta” procedure. While the surgery is generally successful, it is a neurosurgical procedure with the potential for serious complications (meningitis, stroke, permanent facial paralysis, permanent hearing deficit, post-operative blood clots and even death {rare}). Complete cure for HFS occurs in 80% of patients, 10% have marked improved and 10% do not improve.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.