Volume 4 • Issue 2
Eyelid Spasms
Part II – Myokymia and Hemifacial Spasm

by David R. Jordan
M.D., F.A.C.S., F.R.C.S.(C)
INTRODUCTION
There are several different types of eyelid spasms. The three most common are eyelid twitching (myokymia), Essential Blepharospasm, and Hemifacial Spasm.
What causes minor eyelid twitching (myokymia)?
Myokymia is characterized by an involuntary, fine, continuous muscle contraction involving a portion of the orbicularis oculi muscle or other facial muscles. It is often described as a twitch or flickering of the lid. Myokymia is most commonly unilateral, but bilateral cases have been reported. It tends to occur in young, healthy individuals and may last several hours to days. There may be a history of excessive physical exertion, fatigue, lack of sleep, stress, or excess caffeine consumption. A localized oribicularis myokymia may also be seen after almost any type of eyelid surgery.
Myokymia generally requires no treatment as it commonly resolves spontaneously. Obtaining adequate sleep, reducing caffeine intake and decreasing stress are helpful. If the twitches persist on a daily basis for two months or longer, they can generally be abolished with a mild muscle relaxant or an injection of Botulinum toxin (see later). Myokymia that begins with one eyelid, but spreads to include other muscles of the face, requires further investigation.
Surgery
Surgical removal of the eyelid and brow squeezing muscles (myectomy) is available but generally reserved for those not responding to Botulinum toxin injections. The myectomy procedure for the upper lids involves a meticulous dissection and removal of the orbicularis, corrugator and procerus muscles through an eyebrow incision. In some, a lower eyelid myectomy is also required at a later date. The myectomy procedure requires hospitalization for 2 to 3 days. The healing process following a myectomy may take up to a year. In most cases, the patients are able to keep their eyes open immediately following the operation. However, considerable swelling, hematoma, lymphedema, and ecchymosis (varying greatly from patient to patient) may be present early in the post-operative period. Myectomy will improve the visual disability in approximately 90% of cases. Botulinum toxin injections may be required in some patients after the procedure for residual spasms.
The side effects of myectomy include numbness of the forehead, chronic lymphedema (lid swelling), exposure keratitis, ptosis, lid retraction, and ectropion. Most of these problems resolve with time. Only a small number of patients require touch-up procedures.
What is Hemifacial Spasm?
Hemifacial spasm is a benign, uncontrollable twitching of the muscles on one half (hemi-facial) of the face. It is a unilateral facial squeezing disorder unrelated to Essential Blepharospasm. Hemifacial spasms affect only those muscles innervated by the facial nerve. It usually begins around the eye with periodic twitching and spasms of the eyelids that close the eye partially or completely. It slowly spreads to involve other facial muscles on the same side as well as the superficial muscles of the neck (Figures 1a and 1b). The condition does not cause pain but it may with time slowly cause weak ness of the facial muscles involved. Hemifacial Spasm differs etiologically from Essential Blepharospasm. It is most commonly caused by compression of the facial nerve by normal and abnormal vascular structures at the level of the brain stem, ex. a tortuous, distended basilar artery which may be stimulating the facial nerve as well as causing auditory dysfunction. Several different types of benign tumors (ex. dermoid), most commonly occurring outside of the brain but compressing the facial nerve, are the apparent cause in some cases. In other cases, neuroimaging of the brain or even exploratory surgery cannot identify a cause. Although radiographic studies are not of value in investigating patients with Essential Blepharospasm, computed tomography (CT) with use of contrast agents should be performed to look for posterior fossa disease in those patients suspected of having Hemifacial Spasm.
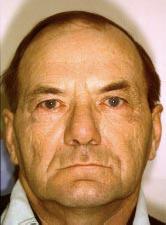
Figure 1a – Pre-spasm.
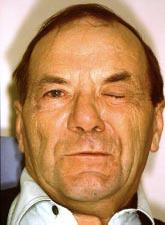
Figure 1b – Half the face is in spasm.
How is Hemifacial Spasm treated?
Hemifacial Spasm may be treated by medication, injection of botulinum toxin or surgery. Drug therapy is usually only of benefit in mild cases and involves the administration of a muscle relaxant such as orphenadrine citrate (Norflex) or baclofen or the anticonvulsant clonazepam (Rivotril).
Botulinum toxin therapy is simple to perform and can be very effective in diminishing the spasms. Unlike Blepharospasms, Hemifacial Spasms seem to have a longer duration of effect with botulinum and may have 4 to 6 months and, occasionally, up to 9 months of relief. The medication is injected into the periocular area as it is with Blepharospasm. It may also be injected over the cheek area to try and decrease some of the lower facial muscle spasms. If the medication is given too close to the mouth, the patient will lose function of the perioral musculature and may have difficulty with talking, chewing food and facial expression.
A neurosurgical microvascular decompression procedure (Janetta procedure) for Hemifacial Spasm may relieve the pressure of the artery on the nerve. Microvascular decompression is a non-destructive procedure which aims to treat the root cause of the disorder, rather than simply treating the symptoms. By separating the causative blood vessels from the nerve, symptoms of Hemi-facial Spasm may be relieved. The operation requires general anesthesia. A small incision is made behind the ear on the affected side and a small opening is made in the bone about the size of a quarter. The area in the brain stem where the 7th nerve is running is visualized with a microscope. The blood vessels are separated from the affected nerve or lateral brain stem. Small implants made of shredded Teflon are used to maintain the separation. The offending blood vessels rest on the Teflon instead of the nerve. The operation takes 2 to 3 hours and the average length of stay in the hospital is 72 hours. While it is generally successful, it is a neuro-logical operation and serious complications are possible (meningitis, stroke, permanent facial paralysis, permanent hearing deficit, post-operative blood clots and even death). These are rare complications. Complete cure for Hemifacial Spasm occurs in 80% of patients, 10% are markedly improved and 10% fail. Recurrence after successful operations is also infrequent with spasms recurring in only 4% to 6% of patients. Although the treatment of Hemifacial Spasm by microvascular decompression involves a neuro-surgical procedure, it is a relatively safe procedure in skilled hands. Operative mortality is negligable and significant morbidity such as hearing loss, stroke, infection or other problems occur in less than 5% of patients. At this point, it remains a safe and well accepted surgical procedure, for those individuals not responding to drugs or botulinum toxin.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.