Volume 11 • Issue 4
Ophthalmic Management of Facial Nerve Paralysis
Part II – Management of the ophthalmic problems

by David R. Jordan
M.D., F.A.C.S., F.R.C.S.(C)
INTRODUCTION
Patients may present to the ophthalmologist with a variety of symptoms associates with facial nerve paralysis that may suggest an etiology. Pain behind the ear or in the mastoid region may accompany facial nerve paralysis. Although this pain is usually associated with the Ramsay Hunt syndrome (or Herpes Zoster), it may also be seen in approximately 50% of patients with Bell’s polsy (usually less intense). If numbness of the face is present, a lesion within the temporal bone or a compressive disorder at the brainstem or cerebellopontine angle should be suspected.
Eye irritation, the commonest ocular symptom, is due to dryness and exposure of the cornea as a result of the diminished tear production, poor blink mechanism, lagophtholmos and lower lid retraction/ectropion.
Immediate attention should be directed toward corneal protection and maintenance of vision. Keeping the cornea lubricated to avoid exposure keratopathy, and potential epithelial breakdown with corneal ulceration is essential. Long-term management of facial disfigurement, tearing, and secondary effects of aberrant regeneration are also important elements in patient care.
Medical Options
Excessive exposure to sunlight is the single most important factor associated with skin cancers on the face, eyelids and arms. Fair skinned people develop skin cancers far more frequently than dark skinned people. Skin cancer may also be hereditary (ex. Basal Cell Nevus Syndrome).
A variety of treatments are available to help keep the cornea moist. Some patients will be fine with one or two of the measures mentioned while others may require several and still remain symptomatic. It is a stepwise progression through the various treatments to find which combination works best. The initial starting point is “artificial tears”.
Artificial tears – are essential to maintain the corneal integrity and should be applied every 2 to 3 hours in the day or more frequently depending on the corneal exposure. There are a variety of basic artificial tears available (“Tears Naturale”, “Genteal”, “Refresh”, “Systane”, as well as many others) that are helpful in patients with mild exposure. “Visene” and other drops that “get the red out” have vasoconstictor agents, which may temporarily relieve the redness but are not helpful in the long term management and may cause more harm than good. In patients with “preservative sensitivity”, preservative free drops are avail-able (e.g. “Cellufresh”, “Tears Bion”, “Artelac”). In those patients with more persistent and severe exposure and not obtaining enough relief with the ‘’basic tears drops” mentioned above, a longer lasting artificial tear (“Tears Naturale Forte”, “Refresh liquigel”, “Celuvisc”) or a ‘’tear gel” (“Tear Gel”, “Genteal Gel”, Liposic Gel” as well as others) may be required. These products simply stay on the surface of the cornea longer.
Lubricating Ointments – are important to use on the exposed cornea at night for corneal protection. Examples include; “Lacrilube ointment”, “Dura tears ointment”, “Hypotears ointment”, “Tears Naturale PM lubricating ointment”. Occasionally ointment is needed during the day but this will significantly blur the vision and is only used in severe cases.
Punctal plugs – were designed to block the tear flow through one of the punctal openings. As a result more of the patients own natural tears are present to add lubrication to the cornea. Current punctal plugs have been designed to sit at the opening of the puncta or more recently sit within the canaliculus itself (Figure 1). This latter variety however cannot be removed easily and may lead to canaliculitis or dacryocystitis with complete nasolacrimal block. Surgery may be required to remove the plug if problems arise. The author does not recommend using the intracanalicular style of plug.

Figure 1 – examples of punctal plugs
Manual lid closure – The patient can manually close the eyelids on the involved side during the day whenever the eye feels irritated or burns.
Taping the eyelids – If the lower eyelid is lax and drooping downward (ectropic), transpore surgical tape (3M company) may be used daily to help pull the lid up and outward toward the lateral orbital rim where the tape is secured. When the eyelid is ectropic, tears easily run over.
When the eyelid is upright and hugging the globe, the tears have a better chance of lubricating the cornea and flowing toward the punctal openings. The palpebral aperature can be further narrowed by limiting the opening of the upper lid. A crescentic piece of tape resembling a half moon can be placed over the tarsal plate in the upper lid. This will prevent the eyelid from opening all the way and improve corneal moisture. Taping the eyelids shut at night with surgical tape or a small Band-Aid may also be helpful to keep the eyelids closed in selected patients.
Patching of the eyelids – can also be done but it is essential to ensure the eyelids are closed under the patch so the patch does not cause further corneal irritation. Commercially available “ophthalmic moisture chambers” (Guibor bubbles from Medtronics) or “swimming goggles” worn at night in addition to lubricating ointment on the cornea may be helpful in some people, to create additional moisture for the cornea. A simple and inexpensive moisture chamber can be made with transparent plastic wrap (Saran wrap) and Vaseline in patients with severe exposure. Patients are instructed to apply lubricating ointment (e.g. lacrilube) to the cornea first and then apply petrolatum ointment (Vaseline) around the orbital rim and lateral nasal bridge. The edges of a 2-inch by 2-inch piece of the Saran wrap are then placed over the ointment to form a seal. A gauze eye patch can be applied over top of this to help keep the saran wrap in place.
Sunglasses – there are several brands of sunglasses avail-able with a foam lining around the rim so that a seal is created between the glass frame and eyelid skin, blocking sun and wind as well as creating a moisture chamber for the cornea (e.g. “Panoptyx” sunglasses). Some patients with both a 5th and 7th nerve paralysis experience photosensitivity that is unrelated to corneal exposure. The photosensitivity is a direct result of the 5th nerve injury (sensory to the cornea) and may be misinterpreted as being due to corneal exposure. In these individuals an FL41 coating can be put on their glasses to help the photosensitivity symptoms in addition to the other lubricating techniques above. The FL41 tint has a rose hue and is applied as a coating to their regular daytime glasses for indoor use or their sunglasses when outside.
Surgical Options
When medical management is unable to maintain corneal integrity or when recovery from facial paralysis is not expected, surgical measures are considered.
Tarsoraphy (suturing the eyelids together)
– may be temporary or permanent depending on the need. A temporary “suture tarsoraphy” can be performed in those patients with severe corneal breakdown and ulceration at anytime to help promote epithelial healing. A 4-0 silk suture from the upper to the lower lid, tied over a cotton, foam or rubber bolster is used to keep the lids closed for 7 to 10 days at a time. If the corneal breakdown does not heal or recurs shortly after the temporary tarsoraphy is taken down despite continuation of artificial tears and lubricating ointment, a more permanent tarsoraphy is performed. A “tarsal pillar tarsoraphy” can be preformed anywhere along the eyelid fissure and is easily reversible. In this technique a vertical strip of tarsus is dissected from the superior eyelid and sutured into a pocket created in the lower eyelid (Fig-ures 2a and 2b). Larger lateral tarsoraphies are occasion-ally required but more unsightly as they shorten the eyelid fissure quite a bit and look un-natural. Medial tarsoraphies are also occaisionally rarely required but avoided if possible as they shorten the eyelid fissure and create a rounded medial canthus appearance.

Figure 2a – temporal tarsoraphy by the “tarsar pillar technique“

Figure 2b – close-up of the tarsal pillar
Tarsoraphy with eyelid tightening
– most of the 7th nerve paralysis patients have some eyelid laxity (as a result of their age) and lower lid retraction (as a result of the paralysed orbicularis oculi muscle). A lower lid tightening procedure (lateral tarsal strip) (Figure 3) in conjunction with a mini lateral tarsoraphy (shortening the eyelid fissure 2 mm) is very effective in restoring the lower eyelid position as well as improving corneal coverage due to a slightly shortened lid fissure.
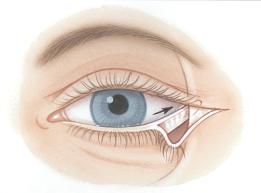
Figure 3– lateral edge of tarsal plate is sutured to lateral orbital rim
Tarsoraphy with lower eyelid spacer grafts (ear cartilage or hard plate grafts) – are occasionally required to elevate the lower lid in those selected patients where a lateral tarsal strip is not enough. This author no longer uses hard palate grafts because of the annoying secretions that can occur from persistant submucosal salivary glands.
Gold weights – a gold weight may be placed in the upper eyelid to help the paralytic eyelid close when the patient blinks. Insertion of a gold weight is a minor procedure performed as an outpatient. The gold weights are available in various weights (0.6 to 1.6 gm). The size of the weight is determined pre-operatively in the office by temporarily taping a trial implant to the lid. (Figure 4a and 4b) The weights are also available in platinum for those sensitive to gold.
Eyelid springs – some surgeons advocate insertion of a stainless steel eyelid spring to help the paralyzed lid close as well as help reanimate the eyelid. The springs, if placed correctly, will help with lid closure but it is difficult to get them to sit just right. In addition, they may require postoperative spring tension adjustment and are prone to extrusion. They are only rarely used.

Figure 4a – lagophthalmos of left upper lid

Figure 4b – a gold weight is being used to help close the eyelid. The gold weight will be placed inside the eyelid surgically once the appropriate weight is determined.
Facial reanimation surgery – can be divided into to “static” and “dynamic” procedures depending upon whether one is trying to re-establish any facial movement.
Brow elevation surgery – is a static procedure and avail-able for those individuals with a great deal of brow droop and dermatochalasis. The brows can be raised by a direct approach adjacent to the eyebrow hair, or a mid forehead approach, temporal hairline approach or endoscopically just behind the hairline. Which technique is done depends on the facial anatomy of the patient.
Lower facial reanimation surgery – is available for long-standing facial paralysis where there is a significant facial droop. There are a variety of static facial slings to elevate the drooping facial muscles back to a more normal position. There are also dynamic facial sling techniques available to try and restore facial animation. A temporalis muscle transfer is one popular technique. The temporalis muscle is dissected out of its fossa and transposed to a new location in the lower face in an attempt to bring motor fibers too the cheeks, upper lip and nasolabial fold area. Although strips of temporalis muscle can also be placed into the upper and lower eyelid to help them close, this technique is not very effective in the eyelid area. Other techniques available to try and restore a dynamic component to the damaged facial nerve include; facial nerve repair with nerve grafting, hypoglossal nerve transfer, microvascualar functional muscle transfer.
Aberrant regeneration and botulinum toxin treatment
Patients who have recovered from Bell’s palsy may have varying amounts of abnormal nerve regeneration (“aberrant regeneration”). This may be manifest as a ptosis of the upper eyelid that is more obvious with talking, eating or chewing. Alternatively, the upper and lower eyelid may partially close, or, there may just be some eyelid flickering due to individual muscle fibers contracting in the eyelid while talking, eating or chewing. In others, when a smile is attempted the eyebrow on the Bell’s palsy side will elevate, or when the individual is asked to close his/her eyelids the corner of the mouth is pulled up. In some patients with aberrant regeneration, they experience tearing while eating, a condition referred to as “crocodile tears”. Botulinum toxin is a simple and effective treatment for some of these aberrant regeneration problems. For example, in those individuals with twitching in the eyelid, an injection of botulinum will eliminate the flickering for 3 to 6 months. Botox is also useful in those with crocodile tears. An injection of botulinum into the lacrimal gland (2-5 units) will eliminate the excess tears for 4-6 months.
Summary
Facial nerve paralysis may arise from a variety of conditions, some benign and some potentially life threatening. Depending on the etiology, the paralysis and facial disfigurement may be temporary or permanent. Immediate attention must be aimed at corneal protection and maintenance of vision; however, long term management of facial disfigurement, tearing, and secondary effects of aberrant regeneration are significant elements in patient care.
If you have any questions regarding the topics of this newsletter, or requests for future topics of InSight, please contact Dr. David R. Jordan office by telephone at (613) 563-3800.